Abstract
Chronic graft versus host disease (cGVHD) is a complex entity and major complication following allogenic hematopoietic stem cell transplantation (allo-HSCT). This study was the first to report oral manifestation and dental management in a patient with cGVHD after allo-HSCT with a longterm follow-up. A 40-year-old man referred to Department of Oral and Maxillofacial Medicine with complaints of tongue burning, mouth dryness, and ulcers. He had chronic myelogenous leukemia and had undergone allo-HSCT. The patient had undergone treatment with several sessions of extracorporeal photopheresis. The GVHD complications had started about nine months after HSCT. In conclusion, the dentist should play a role in the local therapy of cases with oral manifestation and dental management of cGVHD. Controlling the GVHD can reduce oral and dental alterations, increase the improvement of the quality of life, and reduce the need for more intensive immunosuppressive systemic therapies.
Background
Hematopoietic stem cell transplantation (HSCT) is a potentially therapeutic procedure for patients with relapsed or refractory hematological malignancies [1] . Allo-HSCT) is a form of immunotherapy and as an HSCT has increased the survival of patients with relapsed leukemia and high-risk leukemia in remission. Graft versus host disease (GVHD) is one of the most important complaints involving vital organs and infections [2]. The diagnostic criteria of GVHD encompass the signs and symptoms that are complete enough to establish the diagnosis of GVHD, confirmed by local biopsy or diagnostic examinations of other injured organs [3]. Chronic GVHD (cGVHD) is a complex entity and major complication that occur following allo-HSCT [4]. The oral cavity is one of the sites most frequently affected by cGVHD after allo-HCT and can be a significant source of patient morbidity due to both mucosal and salivary gland involvement [5][6]. The development of dental decay is a potentially devastating oral complication that has rarely been reported in the transplantation literature [6]. Herein, we reported oral manifestation and dental management in a patient with cGVHD after allo-HSCT with a long-term follow-up for the first time.
Case History
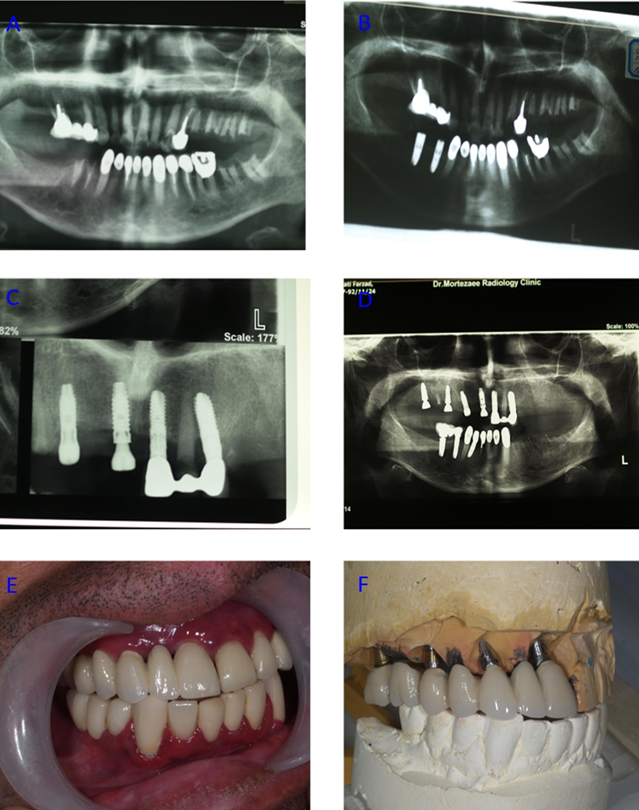
A 40-year-old man referred to the Department of Oral and Maxillofacial Medicine with complaints of tongue burning, mouth dryness, and ulcers on April 13, 2008. In clinical examination, buccal mucosa of the patient was generalized redness and erythema, on both sides of which white plaques with relatively clear areas were seen ( Figure 1A ). The lower lip in vermilion area had shallow ulcers with irregular borders and was surrounded by white plaques ( Figure 1B ). The upper and lower gums had generalized erythema and redness, which induced a desquamative gingivitis ( Figure 1C ). The patient’s history showed he was diagnosed with chronic myelogenous leukemia and underwent allo-HSCT from his sister with blood group B+. The patient was treated with fludarabine and busulfan for a period of 4 to 5 days during HSCT. The genetic similarity of polymerase chain reaction (PCR)-full match led to change of AB+ blood group to B+ 4 to 5 months after HSCT. The GVHD complications started about 9 months after HSCT. After that, cellcept and prednisone (10mg/day) were also added to the previous treatment regimen for 2 years. In the autumn 2007 in Paris, the patient was treated with 15 sessions of extracorporeal photopheresis to control generalized GVHD. In April 2008, the patient referred to the clinic with pain and tongue burning, which showed lichenoid reaction ( Figure 1D ). He was treated with benzydamine mouthwash, betamethasone tab (0.5 mg/day) as mouthwash, and fluconazole capsule (50 mg/day). After one month, the patient referred to the clinic with partial recovery ( Figure 1E ), but yet had complaint of brief burning, so he was treated twice with CO2 laser for 4 min (Power =0.05 watt). Then, he was placed under dental treatments. A post and core with crown were placed for teeth 12 and 13 (1st and 2nd premolars) (with regard to the GVHD, crowns without metal collar were placed) ( Figure 1F , Figure 2A , Figure 2B ). After 2 months, the crown of tooth 25 (central incisor) was broken in the cervical area, which was placed under a post and core with crown without metal collar ( Figure 2C ). At the same time, to prevent the development of cervical caries, the mandibular teeth were also crowned ( Figure 2D , Figure 2E ).
Two years later in 2010, teeth 28, 29, 30, and 31 (1st and 2nd premolars as well as 1st and 2nd molars) were lost ( Figure 2F , Figure 3A ), following which dental implant was proposed. Then, in place of tooth 28 (1st premolar), a fixture (IHDE Dental) with a length of 13mm and width of 3.8 mm and in place of tooth 30 (1st molar), a fixture (IHDE Dental) with a length of 11.5mm and width of 4.5mm were placed ( Figure 3B ). After 6 months, these implants were restored with crown and bridge. Around 3 years later in 2013, because of severe caries due to xerostomia, teeth 3 (1st molar), 5 (1st bicuspid), 6 (cuspid), 7 (lateral incisor), 8 (central incisor), 9 (central incisor), and 10 (lateral incisor) were decayed and fractured. However, the fractures were 4 mm under alveolar bone crest, and crown root ratio was not acceptable, making them to go under implant treatment plan. In place of teeth 8 (central incisor), 6 (cuspid), 4 (2nd bicuspid), and 2 (2nd molar), four fixtures with specifications: (length 13 mm, width 4 mm, TBR system), (length 13 mm width 4 mm, TBR system), (length 13 mm width 4 mm, CMI system), and (length 13mm width 4mm, CMI system) were placed, respectively Figure 3C-F (Some implants were followed for 7 years and some for 4 years). Also, this year the patient was treated with 22 sessions of extracorporeal photopheresis for two months. The patient received cyclosporine (25 mg/day) until August 15, 2016. After this protocol, he did not have any dental problem and chief compliant until January 2018. Then, the patient traveled to another country to continue the treatment. The patient was less likely to have dental extrusion due to oral ulcers and did not cooperate properly. Therefore, control of plaque and oral hygiene due to dry mouth and periodontal ulcer was not well done.
Discussion
Oral GVHD has been described as a possible risk factor for development of oral cancer following allo-HSCT [7]. The primary treatment of GVHD usually consists of therapy with systemic corticosteroids and cyclosporine [8]. This case showed oral and dental treatments in a patient with chronic GVHD with around a 10-year follow-up, which was the longest follow-up in the literature to the best of our knowledge. GVHD is a common complication in HSCT patients ([5][9]). Approximately 80% of cGVHD patients present oral manifestations such as oral ulceration, oral lichenoid lesions, atrophy, and oral mucosa xerostomia [10]-[12]. Oral involvement has been described as a diagnostic sign of cGVHD and one of the first signs or symptoms of the disease [13]. A reduction of 55-90% in saliva flow has been reported in patients with cGVHD, which further exacerbates the consequences of qualitative changes [14]. Because of reduction of saliva, several caries and fractures took place, fracture lines were 4 mm under bone alveolar crest (crown, root ratio was not acceptable), teeth were extracted, and implant was a good choice for this situation [15]. Crowns were zirconium without metal because zirconium ceramics are the most biocompatible materials found [16]. The present case had oral disease, including lichenoid reaction after cGVHD.
One study [6] reported that cGVHD dental caries might be an early and potentially serious oral complication in patients after allo-HSCT. Therefore, patients should be followed carefully after allo-HCT for dry mouth symptoms and routine oral cavity examinations to detect dental changes, including enamel demineralization and frank caries. They should also undergo dental evaluation 6-12 months post allo-HCT and at least every 6 months thereafter. The present case had dental problems after cGVHD for several times, and the teeth of the patient had to undergo implant treatment.
Conclusion
The result showed that the dentist should play a role in local therapy of the cases with oral manifestation and dental management of cGVHD. Therefore, controlling GVHD can reduce oral and dental alterations, improve the quality of life, and reduce the need for more intensive immunosuppressive systemic therapies.
Open Access
This article is distributed under the terms of the Creative Commons Attribution License (CC-BY 4.0) which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
List of abbreviations
cGVHD: Chronic graft versus host disease; Allo-HSCT: allogenic hematopoietic stem cell transplantation; PCR: polymerase chain reaction
Ethics approval and consent to participate
Not to be applied.
Competing interests
The authors declare that they have no conflicts of interest.
Funding
None.
Authors’ contributions
Hamid Reza Mozaffari & Masoud Sadeghi: Literature search, Clinical studies, Data acquisition, Data analysis; Roohollah Sharifi: Manuscript preparation, Manuscript review, Guarantor; Ladan Jamshidy, Neda Omidpanah, Mohammad Shoriabi, & Hedaiat Moradpoor: Concepts, Design, Definition of intellectual content, Literature search, Manuscript editing.
References
-
HR
Mozaffari,
M
Payandeh,
M
Ramezani,
M
Sadeghi,
M
Mahmoudiahmadabadi,
R
Sharifi.
Efficacy of palifermin on oral mucositis and acute GVHD after hematopoietic stem cell transplantation (HSCT) in hematology malignancy patients: a meta-analysis of trials. Wspólczesna Onkologia.
2017;
21
:
299
.
View Article Google Scholar -
M
Payandeh,
M
Sadeghi,
M
Ramezani,
HR
Mozaffari.
The Efficacy of Palifermin on Oral Mucositis and acute GVHD after Hematopoietic Stem Cell Transplantation in Hematologic Malignancy Patients: A Systematic Review and Meta-analysis study. Biomedical Research and Therapy.
2017;
4
:
1676-1692
.
View Article Google Scholar -
SI
Palencia,
JL
Rodríguez-Peralto,
E
Casta-o,
F
Vanaclocha,
L
Iglesias.
Lichenoid nail changes as sole external manifestation of graft vs. host disease. International journal of dermatology.
2002;
41
:
44-45
.
View Article PubMed Google Scholar -
MM
Schubert,
MEP
Correa.
Oral graft-versus-host disease. Dental Clinics.
2008;
52
:
79-109
.
View Article PubMed Google Scholar -
E
Rosa-Garcia,
R
Bologna-Molina,
MT
de Jesús Vega-Gonzalez,
T
de Jesus.
Graft- versus-host disease, an eight case report and literature review. MEDICINA ORAL PATOLOGIA ORAL Y CIRUGIA BUCAL.
2006;
11
:
289
.
-
P
Castellarin,
K
Stevenson,
M
Biasotto,
A
Yuan,
SB
Woo,
NS
Treister.
Extensive dental caries in patients with oral chronic graft-versus-host disease. Biology of Blood and Marrow Transplantation.
2012;
18
:
1573-1579
.
View Article PubMed Google Scholar -
GC
Jaguar,
LP
Kowalski,
DE
da Cruz Perez,
CAL
Pinto,
CM
Esteves,
FA
Alves.
The impact of graft-versus-host disease in the development of oral cancer after allogeneic hematopoietic stem cell transplantation: report of 2 cases. Hematology and Leukemia.
2013;
1
:
4
.
View Article Google Scholar -
A
Dilsiz,
S
Sevinc.
Oral Manifestations in a Patient with Graft Versus Host Disease: A Case Report with a 12-month Follow-Up. Dent.
2014;
2
:
1041
.
-
P
Maturo,
R
Condò,
M
Costacurta,
R
Docimo.
Oral manifestations in the Graft versus Host Disease in paediatric patients: case report. ORAL & implantology.
2009;
2
:
34
.
-
A
Matiakis,
A
Kolokotronis,
D
Antoniades,
A
Asimaki.
Oral involvement in a case of chronic Graft Versus Host Disease. International Journal of Oral-Medical Sciences.
2004;
3
:
105-109
.
View Article Google Scholar -
JAGW
Blajer,
K
Mariusz.
The Inverse Simulation Study of Aircraft Flight Path 8 Reconstruction. Transport.
2002;
XVII
:
103-107
.
-
O
Nicolatou-Galitis,
V
Kitra,
C
Vliet-Constantinidou,
J
Peristeri,
E
Goussetis,
D
Petropoulos,
S
Grafakos.
The oral manifestations of chronic graft-versus-host disease (cGVHD) in paediatric allogeneic bone marrow transplant recipients. Journal of oral pathology & medicine.
2001;
30
:
148-153
.
View Article PubMed Google Scholar -
S
Nakamura,
A
Hiroki,
M
Shinohara,
H
Gondo,
Y
Ohyama,
T
Mouri,
M
Sasaki,
K
Shirasuna,
M
Harada,
Y
Niho.
Oral involvement in chronic graft-versus-host disease after allogeneic bone marrow transplantation. Oral.
1996;
Surgery
:
Oral Medicine
.
View Article Google Scholar -
RM
Nagler,
A
Nagler.
The effect of pilocarpine on salivary constituents in patients with chronic graft-versus-host disease. Archives of oral biology.
2001;
46
:
689-695
.
View Article Google Scholar -
HT
Shillingburg,
S
Hobo,
LD
Whitsett,
SE
Brackett.
Fundamentals of Fixed Prosthodontics, ed, 1997. Learning.
1997;
10
:
40
.
-
A
Alhavaz,
al
Jamshidy L et.
Comparison of the marginal gap of zirconia-fabricated copings generated by CAD/CAM and Copy-Milling methods. Dental Hypotheses.
2015;
6
:
23
.
View Article Google Scholar
Comments

Downloads
Article Details
Volume & Issue : Vol 5 No 6 (2018)
Page No.: 2370-2377
Published on: 2018-06-23
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 9349 times
- Download PDF downloaded - 2099 times
- View Article downloaded - 0 times
 Biomedpress
Biomedpress