Abstract
Background: Psoriasis is a skin inflammation characterized by papules and plaques on the skin surface. Almost 125 million people are affected by psoriasis worldwide. This study aimed to evaluate whether the neutrophil-to-lymphocyte ratio (NLR) can be used as a biomarker for the diagnosis of psoriasis.
Methods: Blood samples of patients with psoriasis and healthy controls were collected for complete blood count testing. A t-test was applied to estimate the difference in the hematological parameters between the two groups.
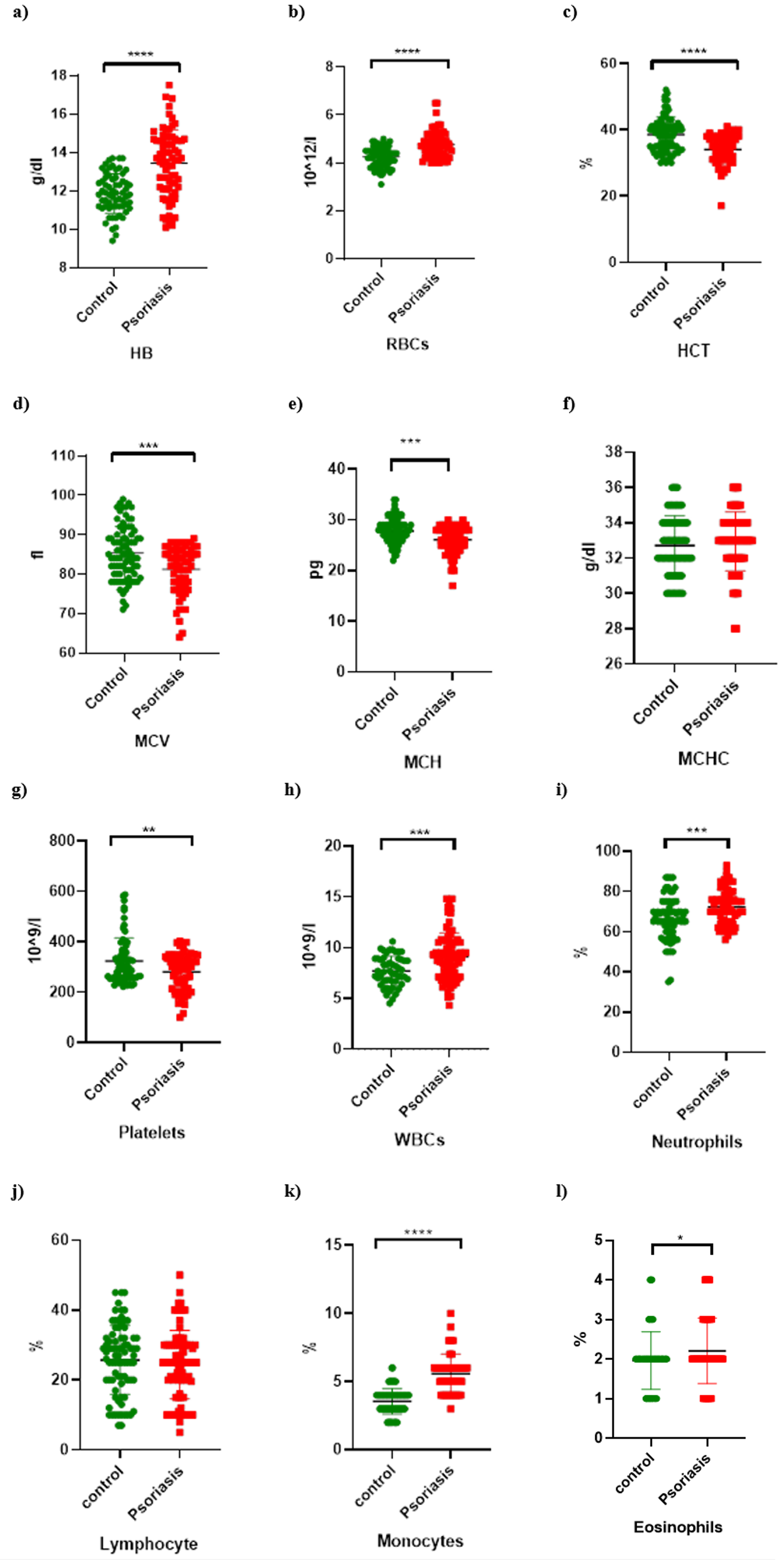
Results: The hemoglobin level (p < 0.0001), hematocrit level (p < 0.0001), red blood cell count (p < 0.0001), mean corpuscular volume (p = 0.0002), platelet count (p = 0.0039), white blood cell count (p = 0.0002), neutrophil count (p = 0.0001), monocyte count (p < 0.0001), and eosinophil count (p = 0.0467) significantly differed between the groups. Meanwhile, the mean corpuscular hemoglobin concentration (p = 0.3989) and lymphocyte count (p = 0.3842) did not. The patients with psoriasis had a higher neutrophil count and a lower lymphocyte count than the healthy controls. The NLR was significantly elevated in the patients with psoriasis.
Conclusion: The NLR is a potential biomarker for the diagnosis of psoriasis.
Introduction
Psoriasis (originating from the Greek word “psora” meaning itch) is a highly stigmatizing and common disease that causes skin inflammation1. It is a prevalent chronic skin inflammatory disease that poses a substantial illness burden equivalent to that of cancer or diabetes2. Hyperproliferation of the epidermis, elongated and conspicuous blood vessels, and thick perivascular lymphocytic infiltration are all symptoms of psoriasis3. Furthermore, it is characterized by papules and plaques on the skin surface that vary in form, location, and severity. They are usually symmetrically distributed in the body folds, scalps, elbows, knees, and lumbosacral area4. The triggering factor of psoriasis is not completely known but is generally believed to have a genetic origin. This disease is aggravated by beta blockers, lithium salt, and other certain medicines5. Its severity is associated with an increased risk of death from a range of causes, the most prevalent of which is cardiovascular death6.
Psoriasis is a public health issue, affecting almost 125 million people worldwide7. Its prevalence varies depending on sex, age, geography, ethnicity, genetics, and environmental variables8. Its incidence ranges between 0.27% and 11.4% in adults. Approximately 2% of the European population is affected with psoriasis9. The prevalence is approximately 3.2% in men and 2.5% in women10. In Spain, psoriasis is common in both men and women, with a prevalence of 1.17–1.43%11. In Norway, the total prevalence is 1.4%, with no sex differences, and individuals aged 30–49 years had the highest prevalence12. In India, psoriasis affects 0.44–2.8% of people in their third or fourth decades of life, with men having a twofold higher risk for this condition than women13.
Variations in several hematological parameters, including the hemoglobin level and platelet count, and different kinds of immune cells have been studied in association with psoriasis. There is either an upregulation or a downregulation in all these parameters regardless of dependency. Blood cell counts, such as the neutrophil-to-lymphocyte ratio (NLR), serve as an additional promising parameter.
An extensive literature survey indicates that no population-based study has yet evaluated the prevalence of psoriasis and its association with hematological parameters in Pakistan. We found a severe shortage of local information in the literature. Almost all information on psoriasis was derived from insubstantial hospital-based studies, and a number of articles were published but not in Pakistan14.
This study aimed to compare the NLR as an inflammatory marker between patients with psoriasis and healthy individuals, evaluate its association with the severity of psoriasis, and determine a cost-effective and easily obtained biomarker for diagnosing this disease.
Methods
Participant selection
Participants were selected from individuals who visited routine medical clinics in Punjab and Islamabad between January and May 2020. Patient recruitment was approved by the ethical committee (UON/ZOO/101) and interdepartmental review board of Pir Mehr Ali Shah Arid Agriculture University, Rawalpindi, Pakistan. Patients were diagnosed by dermatologists as a part of standard clinical care, and no attempt was made to group the participants into different subtypes of the disease.
Blood sampling
Probable sampling was conducted by collecting venous blood samples from 166 participants (83 patients with psoriasis under treatment and 83 healthy controls) after obtaining oral consent. The blood samples were sent to the laboratory for complete blood count (CBC) testing. Different CBC parameters were compiled into a data sheet for further statistical analysis.
Hematological parameter selection
The hematological parameters selected included the hemoglobin level, total red blood cell (RBC) count, hematocrit level, mean corpuscular volume (MCV), mean corpuscular hemoglobin concentration (MCHC), platelet count, white blood cell (WBC) count, neutrophil count, lymphocyte count, monocyte count, and eosinophil count.
Statistical analysis
The statistical analysis was performed using IBM SPSS (version 21.0; license no. Z125-3301-14). Student’s t-test was used for comparing the two groups (case and control). The null hypothesis was that there would be no significant difference in any specific parameter between the groups. Otherwise, an alternative hypothesis was accepted.
| Psoriasis patients | Healthy controls (n = 83) | p Value | |
|---|---|---|---|
| Hb (g/dl) | 12.91 ± 2.25 | 12.57 ± 1.76 | < 0.0001 |
| RBCs (10 12 /l) | 4.64 ± 0.69 | 4.45 ± 0.58 | < 0.0001 |
| HCT (%) | 38.09 ± 6.26 | 38.06 ± 5.53 | < 0.0001 |
| MCV (fl) | 84.01 ± 7.67 | 85.34 ± 6.69 | 0.0002 |
| MCH (pg) | 27.69 ± 3.51 | 27.83 ± 2.54 | 0.0001 |
| MCHC (g/dl) | 32.56 ± 2.43 | 32.60 ± 1.82 | 0.3989 |
| PCT (%) | 332.97 ± 126.17 | 297.02 ± 102 | 0.0039 |
| WBCs (10 9 /l) | 11.36 ± 14.23 | 9.79 ± 3.57 | 0.0002 |
| Neutrophils (%) | 69.43 ± 11.44 | 67.87 ± 11.58 | 0.0001 |
| Lymphocytes (%) | 24.40 ± 9.76 | 26.55 ± 11.02 | 0.3842 |
| Monocytes (%) | 4.66 ± 2.38 | 3.55 ± 0.92 | < 0.0001 |
| Eosinophil (%) | 2.19 ± 1.02 | 2.01 ± 0.84 | 0.0467 |
Results
Incidence of psoriasis according to age
Figure 1 shows the characteristics of the patients with psoriasis and healthy controls in different age groups. Psoriasis was more common among the individuals aged 21 – 30 years. The percentage analysis showed the lowest incidence of psoriasis in the extreme age groups.
Incidence of psoriasis according to sex
Among the 83 patients with psoriasis, the proportion of women (54%) was higher than that of men (46%) (Figure 2).
Hematological parameters
The comparison results of the hematological parameters between the patients with psoriasis and healthy controls are shown in Figure 3. The continuous data described as means ± standard deviations are shown in Table 1. The t-test showed significant differences in the hemoglobin level (p < 0.0001), hematocrit level (p < 0.0001), RBC count (p < 0.0001), MCV (p = 0.0002), platelet count (p = 0.0039), WBC count (p = 0.0002), neutrophil count (p = 0.0001), monocyte count (p < 0.0001), and eosinophil count (p = 0.0467). Meanwhile, the MCHC (p = 0.3989) and lymphocyte count (p = 0.3842) did not significantly differ between the groups (Figure 3 f and j).
NLR
The patients with psoriasis had a significantly higher neutrophil count but a lower lymphocyte count than the healthy controls. The NLR was significantly elevated in the patients with psoriasis compared with that in the healthy controls (Figure 4).
Discussion
Our study demonstrated elevated neutrophil and WBC counts in the patients with psoriasis. Therefore, the neutrophil count can be used as an inflammatory biomarker of psoriasis. Neutrophils are most active during the early phases of inflammation and allow macrophages to heal tissue damage. The expression of numerous cytokines and their receptors coordinates these effects, and these molecules may be used to block certain inflammatory processes15.
Herein, the NLR was elevated in the patients with psoriasis; thus, it can be used as a potential biomarker of this disease. Similar results were obtained in China, in which an elevated NLR was associated with systemic inflammation of psoriasis16. A small-scale cohort study found no significant difference in the NLR between patients and healthy controls but suggested an increased mean platelet volume (MPV) accompanied by a decreased Psoriasis Area Severity Index as a contributing prognostic parameter for the clinical prediction of psoriasis17. An elevated NLR can be caused by various conditions and may be an indicator of a severe inflammatory disorder18. In our study, the NLR was identified as an indicator of systemic inflammation. Similarly, a strong association was previously found between the NLR, platelet count, and MPV and the incidence of psoriasis19. Nevertheless, the platelet count and MPV were less effective predictors of psoriasis than the NLR.
The RBC count was significantly higher in the patients with psoriasis than in the healthy controls in this study. In contrast, patients with psoriasis have been reported to have elevated inflammatory cytokine levels, which increase leukocyte activation products and cause oxidative damage to the components of plasma and erythrocytes20. The erythrocyte count may serve as a long-term indicator of oxidative stress in patients with psoriasis. In the present study, the RBC count was substantially lower in the patients with psoriasis than in the healthy controls. Generally, the RBCs of patients with psoriasis have an increased osmotic fragility, and erythrocytes can reflect the deterioration of psoriasis due to oxidative stress in RBCs21.
In our study, the neutrophil count was significantly higher, and the lymphocyte count was lower in the patients with psoriasis than in the healthy controls. This trend has been recently found in a variety of inflammatory illnesses22. In patients with psoriasis, the lymphocyte count is usually low, and the neutrophil count is high. The presence of reactive platelets in the circulation is indicated by an increase in the platelet volume. Herein, the neutrophil count of the patients with psoriasis was higher when it was tested independently.
Some studies have observed an association of the NLR with other inflammatory disorders. For instance, the NLR has been shown to be a promising diagnostic and prognostic biomarker in the early and late phases of sepsis23, 24. It was also reported to have an acceptable sensitivity in the diagnosis of another systemic inflammation—preeclampsia23, 25. In patients with COVID-19 aged ≥50 years, the NLR is a predictive factor of critical illness26. Recently, a study revealed the diagnostic value of the NLR for psoriasis vulgaris and psoriatic arthritis27.
Neutrophils form extracellular traps that capture and destroy microbes, thus preventing infections. Dysregulation causes systemic inflammation, including psoriasis, rheumatoid arthritis, gout, and autoimmune hepatitis28. Dormant cancer cells can be activated by neutrophil extracellular traps during inflammation29. Taken together, we recommend the NLR as a potential diagnostic and prognostic biomarker for these types of inflammation and cancer.
Conclusions
The neutrophil count is higher, and the lymphocyte count is lower in patients with psoriasis than in healthy individuals. Numerous hematological and biochemical indicators can be used to assess systemic inflammation. The NLR is an emerging marker of inflammation and is elevated in patients with psoriasis. It is considered the most straightforward, accessible, and economical marker for determining inflammation. Therefore, we propose the NLR as a potential biomarker for the diagnosis of psoriasis.
Abbreviations
CBC: Complete Blood Count, HB: Hemoglobin, HCT: Hematocrit test, MCH: mean corpuscular hemoglobin, MCHC: mean corpuscular hemoglobin concentration, MCV: mean corpuscular volume, NLR: Neutrophil to lymphocyte ratio, PTC: Platelet Count, RBCS: Red Blood Cells, WBC: White Blood Cells
Acknowledgments
The authors are thankful to the Vice Chancellor of University of Narowal for providing the platform for the accomplishment of this study.
Author’s contributions
Conceptualization, Supervision and Intellectual Input, MBK, MHA, NS; Methodology and Writing-original draft, BN, MBK, AA, SA, SEH, SSS, MR, FA, RM; Editing and Reviewing, SSS, MBK, FA, RM. All authors read and approved the final manuscript.
Funding
None.
Availability of data and materials
Data is available on request.
Ethics approval and consent to participate
Each participant was asked to sign a written ethical consent form during the interview, before the specimen was taken. The informed ethical consent form was designed and approved by the ethical committee of the University of Narowal, Narowal, Pakistan.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
-
Smith
C.H.,
Barker
J.N.,
Psoriasis and its management. BMJ (Clinical Research Ed.).
2006;
333
(7564)
:
380-4
.
View Article Google Scholar -
Boehncke
W.H.,
Boehncke
S.,
Schön
M.P.,
Managing comorbid disease in patients with psoriasis. BMJ (Clinical Research Ed.).
2010;
340
:
b5666
.
View Article Google Scholar -
de Rie
M.A.,
Goedkoop
A.Y.,
Bos
J.D.,
Overview of psoriasis. Dermatologic Therapy.
2004;
17
(5)
:
341-9
.
-
Langley
R.G.,
Krueger
G.G.,
Griffiths
C.E.,
Psoriasis: epidemiology, clinical features, and quality of life. Annals of the Rheumatic Diseases.
2005;
64
:
ii18-23
.
View Article Google Scholar -
Kim
G.K.,
Del Rosso
J.Q.,
Drug-provoked psoriasis: is it drug induced or drug aggravated?: understanding pathophysiology and clinical relevance. The Journal of Clinical and Aesthetic Dermatology.
2010;
3
(1)
:
32-8
.
-
Abuabara
K.,
Azfar
R.S.,
Shin
D.B.,
Neimann
A.L.,
Troxel
A.B.,
Gelfand
J.M.,
Cause-specific mortality in patients with severe psoriasis: a population-based cohort study in the U.K. British Journal of Dermatology.
2010;
163
(3)
:
586-92
.
View Article Google Scholar -
Griffiths
C.E.,
van der Walt
J.M.,
Ashcroft
D.M.,
Flohr
C.,
Naldi
L.,
Nijsten
T.,
The global state of psoriasis disease epidemiology: a workshop report. British Journal of Dermatology.
2017;
177
(1)
:
e4-7
.
View Article Google Scholar -
Parisi
R.,
Iskandar
I.Y.,
Kontopantelis
E.,
Augustin
M.,
Griffiths
C.E.,
Ashcroft
D.M.,
Global Psoriasis Atlas
National, regional, and worldwide epidemiology of psoriasis: systematic analysis and modelling study. BMJ (Clinical Research Ed.).
2020;
369
:
m1590
.
View Article Google Scholar -
Shaiq
P.A.,
Stuart
P.E.,
Latif
A.,
Schmotzer
C.,
Kazmi
A.H.,
Khan
M.S.,
Genetic associations of psoriasis in a Pakistani population. British Journal of Dermatology.
2013;
169
(2)
:
406-11
.
View Article Google Scholar -
Brandrup
F.,
Green
A.,
The prevalence of psoriasis in Denmark. Acta Dermato-Venereologica.
1981;
61
(4)
:
344-6
.
-
Ferrándiz
C.,
Bordas
X.,
García-Patos
V.,
Puig
S.,
Pujol
R.,
Smandía
A.,
Prevalence of psoriasis in Spain (Epiderma Project: phase I). Journal of the European Academy of Dermatology and Venereology.
2001;
15
(1)
:
20-3
.
View Article Google Scholar -
Braathen
L.R.,
Botten
G.,
Bjerkedal
T.,
Prevalence of psoriasis in Norway. Acta Dermato-Venereologica. Supplementum.
1989;
142
:
5-8
.
-
Thappa
D.M.,
Munisamy
M.,
Research on psoriasis in India: where do we stand?. The Indian Journal of Medical Research.
2017;
146
(2)
:
147-9
.
View Article Google Scholar -
Ejaz
A.,
Suhail
M.,
Iftikhar
A.,
Psoriasis in Pakistani population: Associations, comorbidities, and hematological profile. Journal of Pakistan Association of Dermatologists.
2013;
23
(1)
:
42-6
.
-
Butterfield
T.A.,
Best
T.M.,
Merrick
M.A.,
The dual roles of neutrophils and macrophages in inflammation: a critical balance between tissue damage and repair. Journal of Athletic Training.
2006;
41
(4)
:
457-65
.
-
Wang
W.M.,
Wu
C.,
Gao
Y.M.,
Li
F.,
Yu
X.L.,
Jin
H.Z.,
Neutrophil to lymphocyte ratio, platelet to lymphocyte ratio, and other hematological parameters in psoriasis patients. BMC Immunology.
2021;
22
(1)
:
1-7
.
View Article Google Scholar -
Balevi
A.,
Olmuşçelik
O.,
Ustuner
P.,
Özdemir
M.,
Is there any correlation between red cell distribution width, mean platelet volume neutrophil count, lymphocyte count, and psoriasis area severity index in patients under treatment for psoriasis?. Acta Dermatovenerologica Croatica.
2018;
26
(3)
:
199-205
.
-
Dey
A.K.,
Teague
H.L.,
Adamstein
N.H.,
Rodante
J.A.,
Playford
M.P.,
Chen
M.Y.,
Association of neutrophil-to-lymphocyte ratio with non-calcified coronary artery burden in psoriasis: findings from an observational cohort study. Journal of Cardiovascular Computed Tomography.
2021;
15
(4)
:
372-9
.
View Article Google Scholar -
Pektas
S.D.,
Alatas
E.T.,
Yilmaz
N.,
Plateletcrit is potential biomarker for presence and severity of psoriasis vulgaris. Acta Medica Mediterranea.
2016;
32
(6)
:
1785
.
View Article Google Scholar -
Peluso
I.,
Cavaliere
A.,
Palmery
M.,
Plasma total antioxidant capacity and peroxidation biomarkers in psoriasis. Journal of Biomedical Science.
2016;
23
(1)
:
52
.
View Article Google Scholar -
Arunadevi
D.,
Raghavan
V.,
Nott
A.,
Comparative and Correlative Study of Hematologic Parameters and Selective Inflammatory Biomarkers in Psoriasis. International Journal of Nutrition, Pharmacology, Neurological Diseases.
2022;
12
(1)
:
34
.
-
Hancer
H.S.,
Alatas
E.T.,
Evaluation of mean platelet volume, neutrophil/lymphocyte ratio and platelet/lymphocyte ratio relationship with disease severity and metabolic syndrome in patients with psoriasis vulgaris. Annals of Medical Research.
2020;
27
(10)
:
2503
.
View Article Google Scholar -
Kaushik
R.,
Gupta
M.,
Sharma
M.,
Jash
D.,
Jain
N.,
Sinha
N.,
Diagnostic and Prognostic Role of Neutrophil-to-Lymphocyte Ratio in Early and Late Phase of Sepsis. Indian Journal of Critical Care Medicine : Peer-Reviewed, Official Publication of Indian Society of Critical Care Medicine.
2018;
22
(9)
:
660-3
.
View Article Google Scholar -
Martins
E.C.,
Silveira
L.D.,
Viegas
K.,
Beck
A.D.,
Fioravantti Júnior
G.,
Cremonese
R.V.,
Neutrophil-lymphocyte ratio in the early diagnosis of sepsis in an intensive care unit: a case-control study. Revista Brasileira de Terapia Intensiva.
2019;
31
(1)
:
64-70
.
-
Zheng
W.F.,
Zhan
J.,
Chen
A.,
Ma
H.,
Yang
H.,
Maharjan
R.,
Diagnostic value of neutrophil-lymphocyte ratio in preeclampsia: A PRISMA-compliant systematic review and meta-analysis. Medicine.
2019;
98
(51)
:
e18496
.
View Article Google Scholar -
Liu
J.,
Liu
Y.,
Xiang
P.,
Pu
L.,
Xiong
H.,
Li
C.,
Neutrophil-to-lymphocyte ratio predicts critical illness patients with 2019 coronavirus disease in the early stage. Journal of Translational Medicine.
2020;
18
(1)
:
206
.
View Article Google Scholar -
Nguyen
H.T.,
Vo
L.D.,
Pham
N.N.,
Neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios as inflammatory markers in psoriasis: a case-control study. Dermatology Reports.
2022
.
View Article Google Scholar -
Chiang
C.C.,
Cheng
W.J.,
Korinek
M.,
Lin
C.Y.,
Hwang
T.L.,
Neutrophils in Psoriasis. Frontiers in Immunology.
2019;
10
:
2376
.
View Article Google Scholar -
Albrengues
J.,
Shields
M.A.,
Ng
D.,
Park
C.G.,
Ambrico
A.,
Poindexter
M.E.,
Neutrophil extracellular traps produced during inflammation awaken dormant cancer cells in mice. Science.
2018;
361
(6409)
.
View Article Google Scholar
Comments
Article Details
Volume & Issue : Vol 9 No 9 (2022)
Page No.: 5306-5312
Published on: 2022-09-30
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
- HTML viewed - 4674 times
- PDF downloaded - 1605 times
- XML downloaded - 0 times
 Biomedpress
Biomedpress






