Abstract
There is controversy regarding the role of prior abortion on placenta previa in subsequent pregnancies. We conducted an updated, comprehensive meta-analysis of placenta previa after prior abortion. The search was conducted from PubMed, Web of Science and Scopus databases from the database inception to January 31, 2017. The heterogeneity across studies was evaluated by Q-test and I2 statistical test. Publication bias was assessed by Begg's test and Egger's test. Results of odds ratio (OR) estimates with their corresponding 95% confidence intervals (CI) were pooled using random-effects modeling. The literature search included 872 articles up until January 2017 with 2,134,529 participants. Based on OR estimates obtained from case-control and cohort studies, we found a significant association between prior spontaneous abortions and placenta previa (1.77; 95% CI: 1.60, 1.94) and between prior induced abortions and placenta previa (1.36; 95% CI: 1.02, 1.69). The meta-analysis study herein showed that prior abortion is a risk factor for placenta previa.
Introduction
Placenta previa is defined as the implantation of the placenta in the lower segment of the uterus. It occurs in 3 out of every 1000 pregnancies Findeklee and Costa, 2015. The risk factors for placenta previa are smoking, previous cesarean sections, advanced maternal age, multiparity and conception by in vitro fertilization (IVF) Shobeiri et al., 2017. Abortions have been proposed to be associated with fetal pathology, congenital abnormality, low birth weight and preterm labor in subsequent pregnancies Kashanian et al., 2006.
There is controversy regarding the role of prior abortion on placenta previa in subsequent pregnancies. Some studies have reported an increased risk of placenta previa following abortions Chelmow et al., 1996Eniola et al., 2002Handler et al., 1994Newton et al., 1984ROSE and CHAPMAN, 1986Thom et al., 1992, while others saw no correlation Bakshi et al., 2015Kashanian et al., 2006Latif et al., 2015Usta et al., 2005.
Two previous meta-analyses have shown a positive association between previous abortion(s) and placenta previa in subsequent pregnancies Ananth et al., 1997aFaiz and Ananth, 2003. However, such studies have encountered limitations, such as the limited number of primary databases. Thus, in this study, we performed meta-analysis, based on a larger number of subjects and databases to screen, to address the association of previous abortions and placenta previa. Thus, we conducted an updated and comprehensive meta-analysis of the placenta previa after previous abortion(s).
Materials-Methods
The present meta-analysis study was conducted based on the PRISMA guidelines.
Criteria for including studies
Observational studies (cross-sectional, retrospective and prospective studies) were included in participants declared development of placenta previa following a spontaneous or induced abortion. The following were factors which were excluded in the analysis based on the following criteria: placenta previa following abortion (spontaneous or induced), case report studies, review articles, editorials, and letters or miscellaneous in which full data was not accessible following request from the primary or corresponding authors. The factor of interest was abortion (spontaneous and induced) and the outcome of interest was placenta previa.
Search methods
Two independent authors searched PubMed, Medline and Scopus databases from their time of inception to January 31, 2017. The search terms were conducted based on the following: (placenta previa) and (miscarriage OR induced abortion OR spontaneous abortion OR elective abortion).
After initial evaluation, the studies were independently and carefully evaluated by two authors, and data extraction was performed according to the selection criteria. We extracted the following variables: first author, year of publication, survey years, study country, total sample size, and odds ratio (OR) and their associated 95% confidence intervals (CI). Where discrepancies existed, discussions took place between the two authors until a consensus could be reached.
We assessed the methodological quality of each study independently by two authors via the Newcastle Ottawa Statement Manual (NOS) scale Wells et al., 2012. The scale was from 0 to a maximum of nine stars, and included the following evaluation criteria: selection, comparability, exposure and outcome. Articles scored with seven stars or more were considered high-quality; articles scored with lower stars were considered low-quality Poorolajal and Jenabi, 2016.
Heterogeneity and publication bias
Statistical heterogeneity was determined by the Q statistic test, which was quantified by the I-square values for assessing inconsistency across the studies Higgins et al., 2003. Funnel plot and the Begg's and Egger's tests Begg and Mazumdar, 1994 were used to evaluate the probability of publication bias. Data were analyzed and the outcomes were reported using the random effect model DerSimonian and Laird, 1986. The Stata software, version 13 (StataCorp, College Station, TX) was used for statistical analysis; a statistical significance was set at p< 0.05.
Results
Description of studies
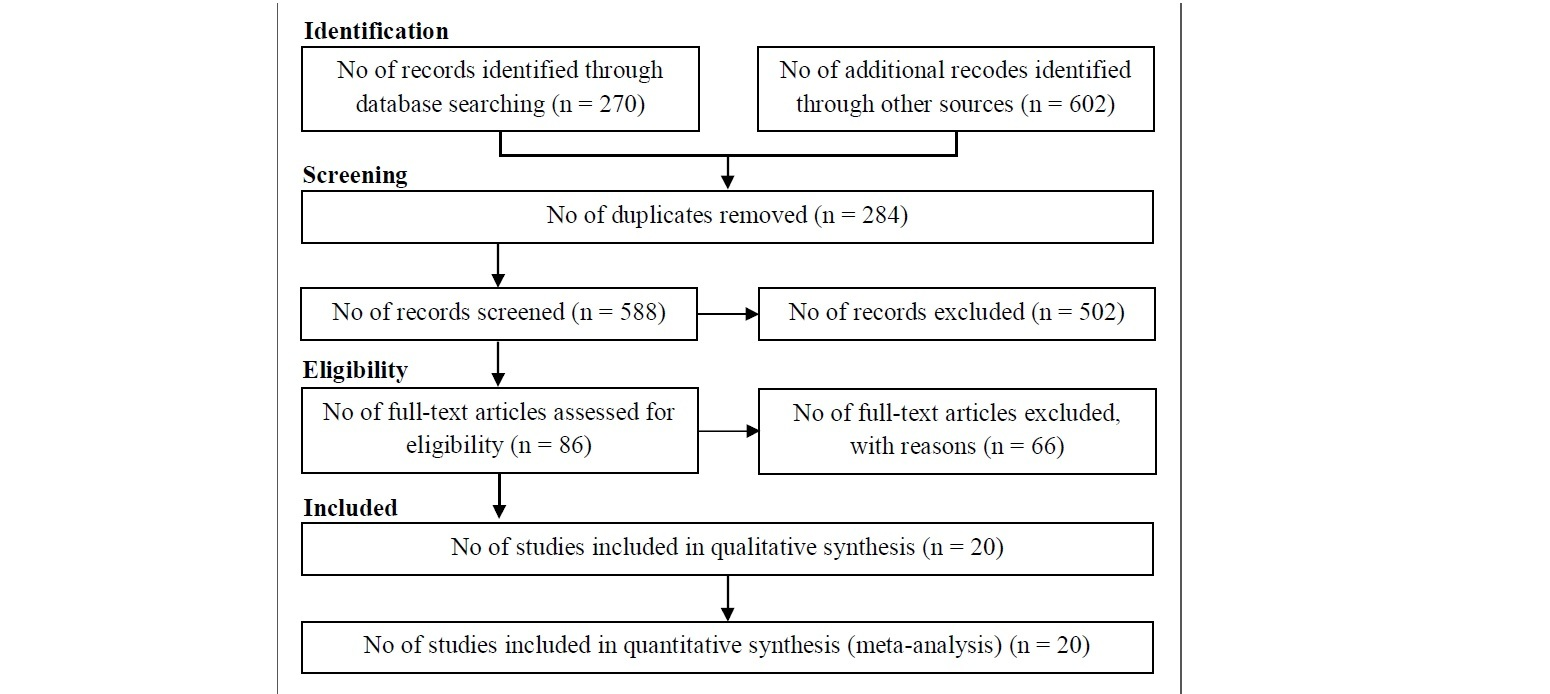
Our search yielded 872 publications of which 20 studies included met inclusion criteria until Jan 2017 ( Figure 1 ). We found 3 cohort studies Bakshi et al., 2015Kashanian et al., 2006Rosenberg et al., 2011 and 17 case-control studies Chelmow et al., 1996Eniola et al., 2002Handler et al., 1994Hung et al., 2007Johnson et al., 2003Kramer et al., 1991Latif et al., 2015Macones et al., 1997Newton et al., 1984ROSE and CHAPMAN, 1986Sheiner et al., 2001Shobeiri et al., 2017Sumigama et al., 2014Taylor et al., 1994Thom et al., 1992Usta et al., 2005Williams et al., 1991 with 2,134,529 participants. All studies were published in English ( Table 1 ).
Effects of exposure
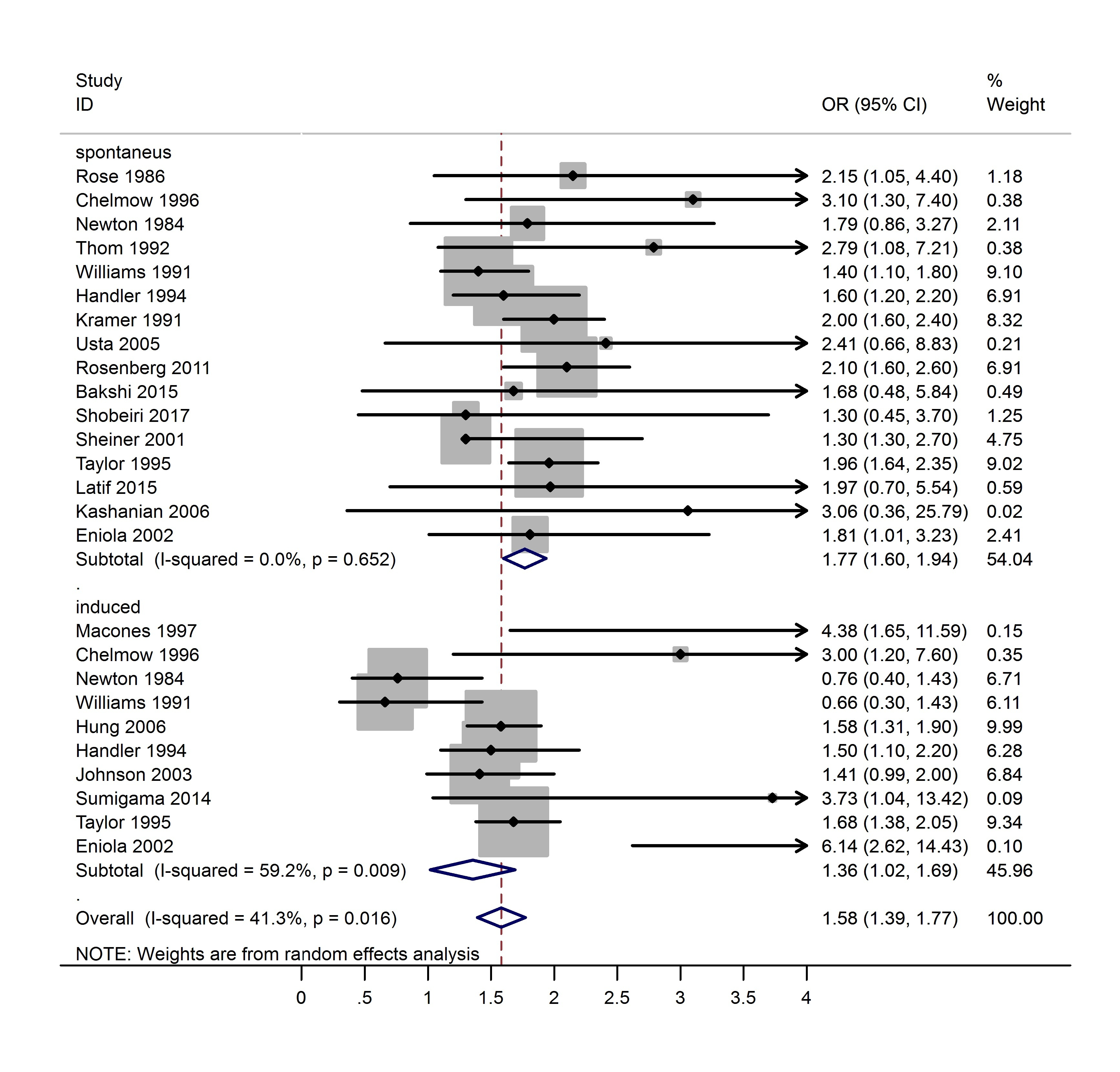
In the present meta-analysis, the association between prior abortion and risk of placenta previa was based on observational studies ( Figure 2 ). Based on OR estimates obtained from case-control and cohort studies, there was a significant association between prior spontaneous abortion and the risk of placenta previa (1.77; 95% CI: 1.60, 1.94) and between prior induced abortion and the risk of placenta previa (1.36; 95% CI: 1.02, 1.69). The results indicated that the measure of the effect was homogenous.
Publication bias
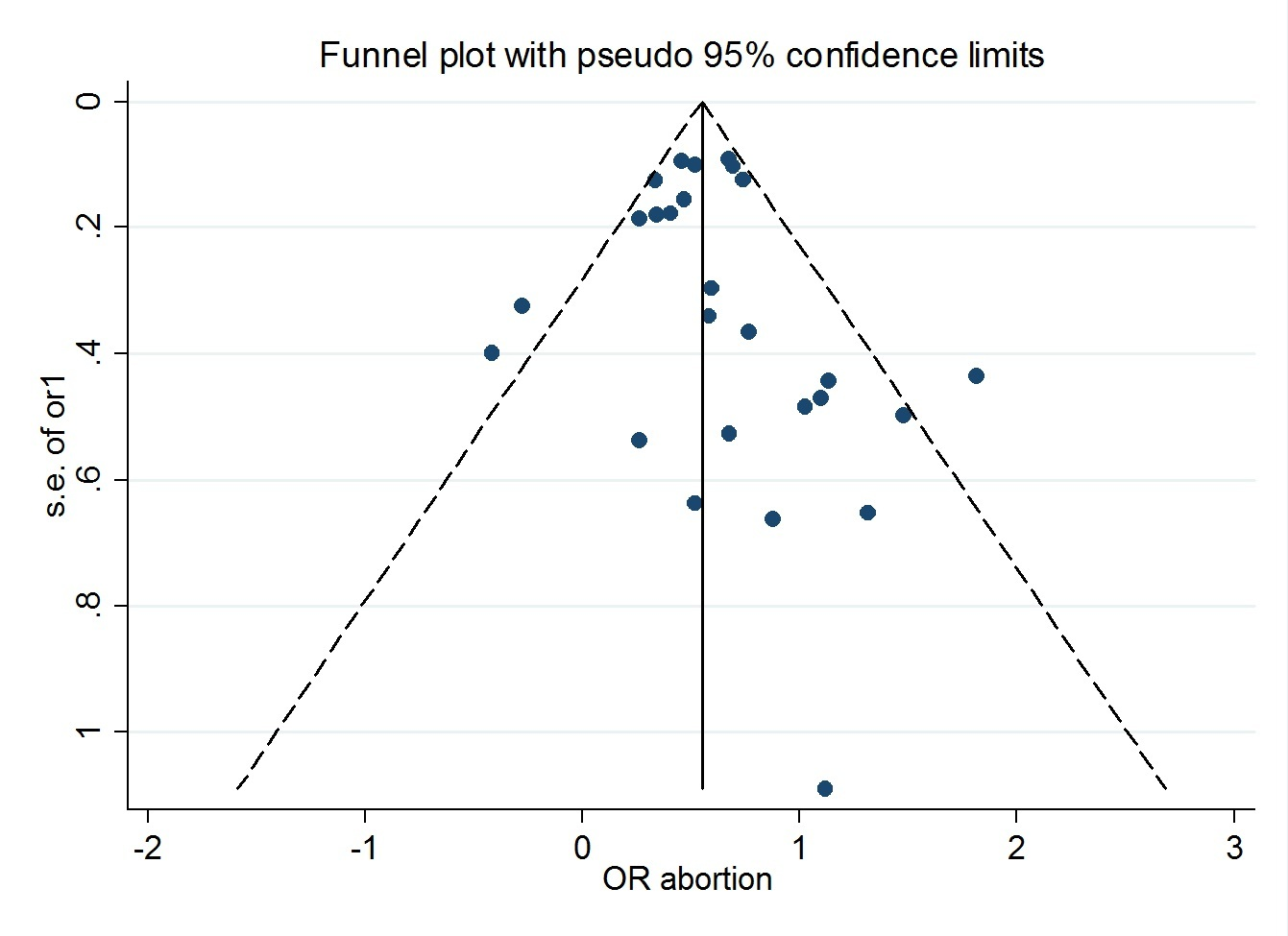
The graphical funnel plots appeared to be symmetrical ( Figure 3 ). The Begg’s (z = 0.90, P = 0.366) and Egger’s test (t = 0.81, P = 0.428) indicated there was no evidence for publication bias.
Quality of the studies
In this meta-analysis, seven studies were of high quality and thirteen studies were of low quality, based on the NOS scale ( Table 1 ).
Discussion
The meta-analysis described herein and based on observational studies show that there is an association between prior abortion and placenta previa. Our results suggest that prior abortion is a risk factor for placenta previa. It has been previously reported that placenta previa is correlated with maternal and fetal complication, such as antenatal and post-partum hemorrhage, preterm delivery, intrauterine growth restriction, malpresentation and poor neonatal outcomes Rombauts et al., 2014.
In a meta-analysis report published by Ananth et al. in 1997 Ananth et al., 1997b, the authors showed that based on OR estimates from all the studies they evaluated, there was a significant increase in the risk of placenta previa after prior spontaneous abortions (1.7; 95% CI: 1.5, 2.0) and after prior induced abortions (1.5; 95% CI: 1.3, 1.7). However, this meta-analysis was limited to eight studies and they searched only the Medline database.
In another meta-analysis, conducted in 2003 by Faiz et al. and which evaluated all articles up to year 2000, the authors showed that prior abortion increased the risk of placenta previa. Based on their results, there was significant association in the increased risk of placenta previa after prior spontaneous abortions (2.0; 95% CI: 1.7, 2.3) and after prior induced abortions (1.5; 95% CI: 1.3, 1.9) Faiz and Ananth, 2003. For their analysis, the authors searched only the Medline database and the meta-analysis included 9 observational studies.
The mechanisms involved in the association of prior abortions and placenta previa is unknown. The damage and scarring to myometrium and endometrium of the uterus during spontaneous and induced abortions may influence the low implantation of placenta in the uterus in subsequent pregnancies Faiz and Ananth, 2003.
The meta-analysis described herein had two limitations. While some studies report only the unadjusted form of OR, we tried to use the adjusted form to control for risk factors which may have impacted the studies included in this meta-analysis. However, doing so might introduce information bias in our results. Also, in the present study, we attempted to identify all published studies. However, in spite of our efforts, we could not find two studies that might have reported data on placenta previa. Despite these limitations, the present meta-analysis study was drawn from a large sample size; the 20 studies should efficiently estimate the association between prior abortion and risk of placenta previa. Our results indicate, based on odds ratio reports in epidemiological studies, that prior abortion (spontaneous and induced) can increase the risk of placenta previa.
Conclusion
We showed based on our present meta-analysis of observational studies that prior spontaneous and induced abortions can increase the risk of placenta previa. Therefore, prior abortion is a risk factor for placenta previa.
Author contribution
EJ and MK designed the study and processed the data. MK and EJ performed the statistical analysis. EJ and MK interpreted the results and wrote the first draft. Two authors read and approved the final manuscript.
References
-
C.V.
Ananth,
W.A.
Bowes,
D.A.
Savitz,
E.R.
Luther.
Relationship between pregnancy-induced hypertension and placenta previa: a population-based study. American journal of obstetrics and gynecology.
1997a;
177
:
997-1002
.
-
C.V.
Ananth,
J.C.
Smulian,
A.M.
Vintzileos.
The association of placenta previa with history of cesarean delivery and abortion: a metaanalysis. American journal of obstetrics and gynecology.
1997b;
177
:
1071-1078
.
-
K.
Bakshi,
T.U.
Rani,
P.P.
Kumar,
G.
Prabhakar.
Risk of adverse pregnancy outcomes after prior spontaneous abortion. Current Medicine Research and Practice.
2015;
5
:
258-261
.
-
C.B.
Begg,
M.
Mazumdar.
Operating characteristics of a rank correlation test for publication bias. Biometrics.
1994;
:
1088-1101
.
-
D.
Chelmow,
D.E.
Andrew,
E.R.
Baker.
Maternal cigarette smoking and placenta previa. Obstetrics & Gynecology.
1996;
87
:
703-706
.
-
R.
DerSimonian,
N.
Laird.
Meta-analysis in clinical trials Control Clin Trials 7: 177-188. Find this article online.
1986
.
-
A.
Eniola,
A.
Bako,
D.
Selo-Ojeme.
Risk factors for placenta praevia in southern Nigeria. East African medical journal.
2002;
79
:
536-538
.
-
A.
Faiz,
C.
Ananth.
Etiology and risk factors for placenta previa: an overview and meta-analysis of observational studies. The Journal of Maternal-Fetal & Neonatal Medicine.
2003;
13
:
175-190
.
-
S.
Findeklee,
S.
Costa.
Placenta Accreta and Total Placenta Previa in the 19th Week of Pregnancy. Geburtshilfe und Frauenheilkunde.
2015;
75
:
839-843
.
-
A.S.
Handler,
E.D.
Mason,
D.L.
Rosenberg,
F.G.
Davis.
The relationship between exposure during pregnancy to cigarette smoking and cocaine use and placenta previa. American journal of obstetrics and gynecology.
1994;
170
:
884-889
.
-
J.
Higgins,
S.
Thompson,
J.
Deeks,
D.
Altman.
Measuring inconsistency in meta-analyses BMJ 327: 557-560. Find this article online.
2003
.
-
T.H.
Hung,
C.C.
Hsieh,
J.J.
Hsu,
T.H.
Chiu,
L.M.
Lo.
Risk factors for placenta previa in an Asian population. International Journal of Gynecology & Obstetrics.
2007;
97
:
26-30
.
-
L.
Johnson,
B.
Mueller,
J.
Daling.
The relationship of placenta previa and history of induced abortion. International Journal of Gynecology & Obstetrics.
2003;
81
:
191-198
.
-
M.
Kashanian,
A.
Akbarian,
H.
Baradaran,
S.
Shabandoust.
Pregnancy outcome following a previous spontaneous abortion (miscarriage). Gynecologic and obstetric investigation.
2006;
61
:
167-170
.
-
M.D.
Kramer,
V.
Taylor,
D.E.
Hickok,
J.R.
Daling,
T.L.
Vaughan,
K.A.
Hollenbach.
Maternal smoking and placenta previa. Epidemiology.
1991;
:
221-223
.
-
L.
Latif,
U.J.
Iqbal,
M.U.
Aftab.
Associated risk factors of placenta previa a matched case control study. Pakistan Journal of Medical and Health Sciences.
2015;
9
:
1344-1346
.
-
G.A.
Macones,
H.M.
Sehdev,
S.
Parry,
M.A.
Morgan,
J.A.
Berlin.
The association between maternal cocaine use and placenta previa. American journal of obstetrics and gynecology.
1997;
177
:
1097-1100
.
-
E.R.
Newton,
V.
Barss,
C.L.
Cetrulo.
The epidemiology and clinical history of asymptomatic midtrimester placenta previa. American journal of obstetrics and gynecology.
1984;
148
:
743-748
.
-
J.
Poorolajal,
E.
Jenabi.
The association between body mass index and preeclampsia: a meta-analysis. The Journal of Maternal-Fetal & Neonatal Medicine.
2016;
29
:
3670-3676
.
-
L.
Rombauts,
C.
Motteram,
E.
Berkowitz,
S.
Fernando.
Risk of placenta praevia is linked to endometrial thickness in a retrospective cohort study of 4537 singleton assisted reproduction technology births. Human Reproduction.
2014;
29
:
2787-2793
.
-
G.L.
ROSE,
M.G.
CHAPMAN.
Aetiological factors in placenta praevia a case controlled study. BJOG: An International Journal of Obstetrics & Gynaecology.
1986;
93
:
586-588
.
-
T.
Rosenberg,
G.
Pariente,
R.
Sergienko,
A.
Wiznitzer,
E.
Sheiner.
Critical analysis of risk factors and outcome of placenta previa. Archives of gynecology and obstetrics.
2011;
284
:
47-51
.
-
E.
Sheiner,
I.
Shoham-Vardi,
M.
Hallak,
R.
Hershkowitz,
M.
Katz,
M.
Mazor.
Placenta previa: obstetric risk factors and pregnancy outcome. Journal of Maternal-Fetal Medicine.
2001;
10
:
414-419
.
-
F.
Shobeiri,
E.
Jenabi,
M.
Karami,
S.
Karimi.
Determinants of placenta previa: a case-control study. Biomedical Research and Therapy.
2017;
4
:
1411-1419
.
-
S.
Sumigama,
C.
Sugiyama,
T.
Kotani,
H.
Hayakawa,
A.
Inoue,
Y.
Mano,
H.
Tsuda,
M.
Furuhashi,
O.
Yamamuro,
Y.
Kinoshita.
Uterine sutures at prior caesarean section and placenta accreta in subsequent pregnancy: a case-control study. BJOG: An International Journal of Obstetrics & Gynaecology.
2014;
121
:
866-875
.
-
V.M.
Taylor,
M.D.
Kramer,
T.L.
Vaughan,
S.
Peacock.
Placenta Previa and Prior Cesarean Delivery: How Strong is the Association?. Obstetrics & Gynecology.
1994;
84
:
55-57
.
-
D.H.
Thom,
L.M.
Nelson,
T.L.
Vaughan.
Spontaneous abortion and subsequent adverse birth outcomes. American journal of obstetrics and gynecology.
1992;
166
:
111-116
.
-
I.M.
Usta,
E.M.
Hobeika,
A.A.A.
Musa,
G.E.
Gabriel,
A.H.
Nassar.
Placenta previa-accreta: risk factors and complications. American journal of obstetrics and gynecology.
2005;
193
:
1045-1049
.
-
G.
Wells,
B.
Shea,
D.
O’Connell,
J.
Peterson,
V.
Welch,
M.
Losos.
The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa, Ontario, Canada: Ottawa Hospital Research Institute.
2012;
2013
.
-
M.A.
Williams,
R.
Mittendorf,
E.
Lieberman,
R.R.
Monson,
S.C.
Schoenbaum,
D.R.
Genest.
Cigarette smoking during pregnancy in relation to placenta previa. American journal of obstetrics and gynecology.
1991;
165
:
28-32
.
Comments
Downloads
Article Details
Volume & Issue : Vol 4 No 07 (2017)
Page No.: 1441-1450
Published on: 2017-07-28
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
- HTML viewed - 14587 times
- Download PDF downloaded - 2238 times
- View Article downloaded - 10 times
 Biomedpress
Biomedpress