Abstract
Background: The aim of the present study is to evaluate the effects of laughter yoga exercises on anxiety and sleep quality in patients suffering from Parkinson's disease.
Methods: In the study a semi-empirical and applied research design was used, which involved a pre-test and post-test, and appropriate control group. The study consisted of 24 patients suffering from Parkinson's disease who were referred and admitted to Hazarate Raoul Allah Hospital in Tehran, Iran. The patients ranged in age from 55 to 75 and met the study criteria prior to entering the research study. The patients were randomly divided into two groups: control or experimental (n=12 per group). After completing exercises (laughter yoga), post-evaluation of anxiety and sleep quality of patients in both groups were conducted using questionnaires. For normalization of research data, the Mann-Whitney nonparametric test was used. Statistical analyses were conducted using the SPSS software, with the statistically significant level set at P < 0.05.
Results: The Mann-Whitney tests indicated that there was a significant difference between the average stress change as well as sleep quality in patients suffering from Parkinson's disease (versus control subjects) following laughter yoga exercises. Indeed, regarding sleep quality laughter yoga was only effective on the subjective quality of sleep and latency in sleeping. There was no observation of a significant effect on the duration of sleep, sleep efficiency, sleep disturbances, use of sleeping pills, or daily functions of the patients.
Conclusion: The results of the present study demonstrate that laughter yoga exercises can reduce anxiety and improve sleep quality in patients suffering from Parkinson's disease. As a result, laughter yoga exercises may be beneficial as a complementary therapy with standard treatment methods to reduce anxiety and improve sleep quality in patients with Parkinson's.
Introduction
Parkinson’s disease is a chronic and progressive central nervous system disorder. It is classified among the motor system disorders Yektamaram, 2010 which mostly affects elderly individuals Yousefi, 2010 and is a common cause of disability in this age group Afshar and Ghandehari, 2006. Movement disorders are neurological conditions which affect the control of movements. Activities such as walking or sipping a cup of tea may be difficult. In some cases, people cannot relax their bodies and some parts of their body remain in constant motion Emsaki, 2010. British doctor James Parkinson was the first to describe the disease in 1817; he called the disease "shaking paralysis" and today it is known as Parkinson's disease Abedzadeh, 2012.
In 1960, researchers found that the cause of this disease is a dysfunction in a particular area of the brain. Notably, the brain is unable to produce the chemical substance dopamine, a neurotransmitter which controls body muscle activities Yektamaram, 2009. Generally, Parkinson's disease occurs because of the reduction or loss of a major part of the nerve cells that produces dopamine in the region of the brain called the substantia nigra. Without dopamine, the brain cannot send motor messages Yektamaram, 2010 leading to bradykinesia, tremors, mental deterioration and other dysfunctions of the automatic nervous system Najarian, 2008.
Furthermore, psychological problems such as depression, anxiety, self-doubt, sleep disturbance, fear and shame can result from Parkinson's disease Abedzadeh, 2012. Parkinson's disease has been seen in patients worldwide, affecting all ethnic groups and social classes Moshfeghi, 2010. While many studies estimate the prevalence of the disease to be similar for men and women, some have reported it to be slightly more common (3:2 ratio) in men than women Abargouei Azizi, 2011. The cause of this disease is still not fully understood but reports suggest an association with genetic factors (to a lesser extent) and environmental factors (to a greater extent), including agricultural jobs, drinking well water, village life and exposure to pesticides Huang et al., 2014.
The main neuropathological sign of Parkinson’s disease is destruction of dopamine-producing cells in the substantia nigra of the mid-brain. The decrease of dopamine levels and subsequent disruption of balance of dopamine and acetylcholine gives rise to a variety of movement disorders Hartmann, 2005. In fact, clinical signs (e.g. movement disorders) of the disease are observable when loss of about 80% of dopamine-producing cells in the mid-brain occurs and when neurotransmission in the basal ganglia of the brain is disrupted. The most prominent movement dysfunctions of Parkinson's patients are reduced balance, loss of balance, lack of postural control and progressive reduction in the speed and range of motion Morris, 2000. With an increased risk of falling, elderly patients with Parkinson’s are prone to fractures, dislocations and serious soft tissue damages Robinson et al., 2005. In terms of physiology, the “balance” referred to above is defined as the interaction between levels of control mechanisms of balance; with respect to biomechanics, the “balance” is defined as the ability to maintain and return the center of gravity of the body within a stability that is determined by the base of support Bellew et al., 2003. Postural instability, thus, can occur as a result of decreased muscle strength and in combination with other complications which result from the destruction of dopamine-producing cells in the basal ganglia Tinetti, 2003.
Researchers have suggested that the main cause of balance problems in Parkinson’s patients is the impairment of excitation/inhibition in the basal ganglia (which also impacts downstream effects through direct and indirect means) Shannon, 2004. On the other hand, being sick and/or elderly can increase the complications of this disease Dibble et al., 2006. With the onset of old age, changes occur in the musculoskeletal system, vestibular system, sensory system and visual system. The changes in the metabolic and physiological systems involved in balance can put elderly individuals at risk for serious injuries related to lack of balance, including fractures and long-term disabilities.
Researchers have categorized factors which affect postural control deficits in older adults into two categories: external (foreign) and internal (domestic) factors. External factors can be uneven ground and use of inappropriate shoes. Internal factors include dysfunctions of the physiological systems of the body (e.g. decreased muscle strength, decreased range of motion, and/or reduction of visual, vestibular and proprioceptive senses) Giroux, 2007Lord, 2003. Thus, aging and inactivity may lead to enhanced aggravation of primary and secondary symptoms in patients. There is abundant evidence which show that the number of falls by Parkinson’s patients is significantly higher than those for healthy, elderly individuals Nelson et al., 2002.
At present, elderly people constitute 7% of the population. Within the next 20 years, this percentage will expected to double; in 30-40 years the majority of the population will be elderly people Heydari et al., 2010. With the elderly population expected to rise dramatically worldwide, so too is the number of patients expected to suffer from Parkinson’s disease Giroux, 2007. Due to the progressive process of Parkinson's disease in the absence of controls, everyday problems of these patients will be increased and the tangible outcomes are movement disorders, psychological problems and economic problems for society Abargouei Azizi, 2011Morris, 2000.
Depression and anxiety are two times more likely to occur in individuals recently affected by Parkinson's disease than in healthy individuals. The tremors and movement disorders caused by Parkinson's are well-known, but the disease actually begins in the brain, affecting various chemical compounds which trigger, initially, sleep dysfunctions and mild forms of depression. In fact, sleep disorders are commonly seen in patients suffering from Parkinson's disease. Studies show that the prevalence of sleep disorders in Parkinson's disease is 60 to 98% Covassin et al., 2012. This figure is higher than the prevalence of this disorder in people not suffering from Parkinson's disease in the same age and sex demographics Scheller et al., 2008.
Parkinson's patients often experience sleep disturbances, excessive daytime sleeping, delay in falling asleep, and difficulty in maintaining sleep Iranzo de RA, 2011. In addition, pulmonary disorders during sleeping, restless legs syndrome, mood and behavioral disorders, and rhythmic leg movements in sleep are common problems in the patients Margis et al., 2009. Despite the obvious sleep disorders in these patients, studies have rarely addressed or evaluated them Naismith et al., 2010. To date, various questionnaires have been prepared to assess the presence or absence of sleep disorders in order to provide treatment guidance. Indeed, treatment of non-motor disorders can improve the patient's quality of life Najafi et al., 2012. The cause of insomnia in Parkinson's disease is multifactorial and includes older age, nocturnal motor symptoms, psychological disorders (including depression and hallucinations), and pharmacological effects.
The relationship between Parkinson’s disease and severity of sleep disturbance has been studied and reported Najafi et al., 2012. However, another study evaluating sleep quality in patients suffering from Parkinson's disease showed no significant correlation between the disease and duration or severity of sleep disturbance Moshfeghi, 2010. In another study, sleep tests on patients with Parkinson's disease were conducted; the study conclusion was that the most common symptoms in these depressed patients were turmoil (43.2%), anxiety (43.3%), and irritability (40.1%) Abedzadeh, 2012. Patients suffering from Parkinson's disease often experience feelings of anxiety or fear of attacks. Mood changes may also occur due to changes in drug levels Soleimani, 2015. The most obvious manifestation of mental problems in patients suffering from Parkinson's disease is anxiety and depression, which are caused by physical symptoms and the resulting limitations associated with those. Tremors, slow movements and difficulty of movement can cause social isolation of the patient. Abnormal gait, trapped legs while walking, falling, problems with speech, and change in the patient’s voice can all create a feeling of embarrassment in the patient, thereby reducing their motivation and willingness to participate in social activities Pierce, 2008. Overall, these factors can affect the patient’s quality of life. However, use of complementary therapies in combination with standard therapies may improve quality of life of individuals with Parkinson’s.
In addition to drug therapy, exercise and physical activity can be used as complementary therapies Keykhai Hosseinpour, 2013. Participation in sports is a beneficial means to achieve health and well-being. Engagement in exercise leads to physical, mental and social health. Indeed, physical activity/exercise is one of the main ways to prevent, delay or treat problems caused by the aging process, and has a profoundly positive impact on improving the quality of life of elderly people Khorsand, 2016Shaumway cook, 2007.
Of the exercises, “laughter yoga” is a relatively new complementary therapy with beneficial effects. Laughter yoga was invented in 1995 by a Hindi physician named Madan Katarya. It combines the standard yoga breathing exercises with laughing exercises, and includes a variety of fun sports too Pezeshki, 2012. Laughter is an emotional reaction that affects human life and social life in a positive manner, and has characteristics that distinguish it from other emotional reactions Pezeshki, 2012.
Extensive research from the past two decades across various countries has proven that laughter has a positive effect on the body and is involved in strengthening the immune system. Scientists have also found that laughter has a preventive and therapeutic value Kataria, 2004. Laughter yoga includes mind-body techniques and combines different methods of laughing with breathing exercises Hasan and Hasan, 2009Keykhai Hosseinpour, 2013. People who are regularly practicing laugh yoga exercises have experienced improvements in their health, mental outlook and energy level Pezeshki, 2012.
Studies have shown that when someone pretends to laugh or be happy, the body produces chemicals (e.g. dopamine, serotonin, etc.) that induce a state of happiness Kataria, 2004. Thus, the laughter is powerful in inducing physiological changes in the body. According to the principle “motion creates emotion”, if one puts his/her body in a state of happiness, the mind will follow to a happy state Kataria, 2004. Currently, the increase in population of elderly people (due to a reduction in birthrate, improvement of health and increased life expectancy) has garnered greater focus on the problems of the elderly Abedzadeh, 2012.
Aging is a natural and inevitable process that affects all biological and psychological aspects of humans. Growth and maturity are the center point of childhood and youth hood. During adulthood, particularly during middle age and elderly age, most physical and mental functions decrease or atrophy due to aging. However, a sedentary lifestyle also accelerates the aging process.
Physical, psychological, social and economic problems in old age often increase by 2-fold Abedzadeh, 2012. Due to the growing elderly population in the world, according to estimates by the mid-21st century the number of the elderly is projected to reach 3.1 billion. Thus, it is critical to find solutions to health issues (e.g. Parkinson’s disease) of this important age demographic.
Due to the close relationship between body and mind, it is clear that declining physical abilities along with increasing social/economic problems in old age can create a fertile ground for physical and mental illnesses. Parkinson's and Alzheimer's are among the most common diseases. Although the motor ability of patients is affected, they predominantly suffer from cognitive and behavioral impairment. Depression, dementia and mental disorders have a major impact on the quality of life for both patients and their families Abedzadeh, 2012.
Laughter yoga, through release of neurotransmitters from brain cells, can help induce feelings of happiness and potentially alleviate depression. According to modern medicine, disease originates from our minds (i.e. emotional thoughts and overall state of mind). Accordingly, it may be very beneficial to do laughter yoga exercise programs as a complementary step to treat the well-being of patients suffering from Parkinson’s Keykhai Hosseinpour, 2013.
Generally, the treatment of Parkinson's disease consists of three parts: surgery, medication and rehabilitation. Following selection of treatment plan, a detailed history of disease and clinical or para-clinical evaluations are conducted. Based on review of the literature on the role of treatment options for mental disorders in people with Parkinson’s, the interventions/treatments are mainly pharmaceutical, nutritional and physiological; the role of physical activities and different sport activities in the treatment of Parkinson’s have been less studied Abedzadeh, 2012. As aforementioned, laughter exercises can impact organs and muscles, strengthen the immune system, induce blood biochemical changes, and affect oxygen; all of these play a significant role in the potential prevention and treatment of Parkinson’s disease Pezeshki, 2012. Therefore, we postulated that problems (e.g. depression, anxiety, loss of confidence, and sleep disorders) experienced by Parkinson’s patients may be improved by laughter yoga exercises as a complementary treatment. We hypothesized that a course of laughter yoga exercises might improve anxiety and sleep quality of patients suffering from Parkinson’s disease.
This study aimed to determine the effect of laughter yoga exercises on the severity of anxiety in patients with Parkinson's disease; and to determine the effect of laughter yoga exercises on sleep quality of patients with Parkinson's disease.
Materials-Methods
Methodology
This study was done with the purpose of studying a course of laughter yoga exercises on anxiety and sleep quality of patients suffering from Parkinson’s.
Patients
For the present study there were initially 30 Parkinson’s patients who were referred to Hazarate Raoul Allah hospital in Tehran, Iran. Patients ranged in age from 55 to 75 years old and each met the study requirements before entering into the research study.
Groups of investigation
Parkinson’s disease is classified as Stage 1, 2 or 3, according to the Hoehn and Yahr Scale (H&Y). Parkinson’s patients without chronic heart and respiratory disease, without open surgery in the inner region in the last six months, and without high blood pressure who voluntarily participated in this study were randomly divided into two groups of 15. One group was the experimental group (laughter yoga exercises) and the other was the control group (no laughter yoga exercises). From those individuals, 6 were removed from the study due to lack of continuous training, setting the machine Deep brain stimulation (DBS), and withdrawal for work purposes. After exclusion of these 6 patients, the final study consisted of 12 patients in the experimental group and 12 patients in the control group.
The voluntary participation of Parkinson’s patients as subjects in the study was reviewed and approved by physicians. Notably, before the study was initiated subjects from both groups agreed by written consent to participate in the research study; those in the appropriate group(s) agreed to engage in laughter yoga classes. Also, before the start of the study, all executive items were approved by a committee of the University University Research Committee (Islamic Azad University of Karaj).
Laughter yoga exercises
Firstly, as a pre-test, the anxiety and sleep quality of patients suffering from Parkinson’s disease in both the experimental and control groups, were measured by the anxiety inventory of Beck (1988) and the sleep quality inventory of Pitezbourg (1989) (PSQI), respectively. Then the treatment group, in addition to standard medical treatment, performed laugher yoga exercises under the supervision of a laughter yoga instructor for 8 weeks (2 sessions per week, 45 minutes per session). Meanwhile, patients in the control group received their standard medical treatment and continued their typical daily activities but did not practice any laughter yoga exercises.
Statistical analysis
After completing the laughter yoga exercises, as a post-test, the anxiety and sleep quality of the patients in both experimental and control groups were measured using questionnaires. To normalize the research data, the Mann-Whitney nonparametric test was used. As well, all the analyses was done at a significance level of (P<0.05) using SPSS software.
Results
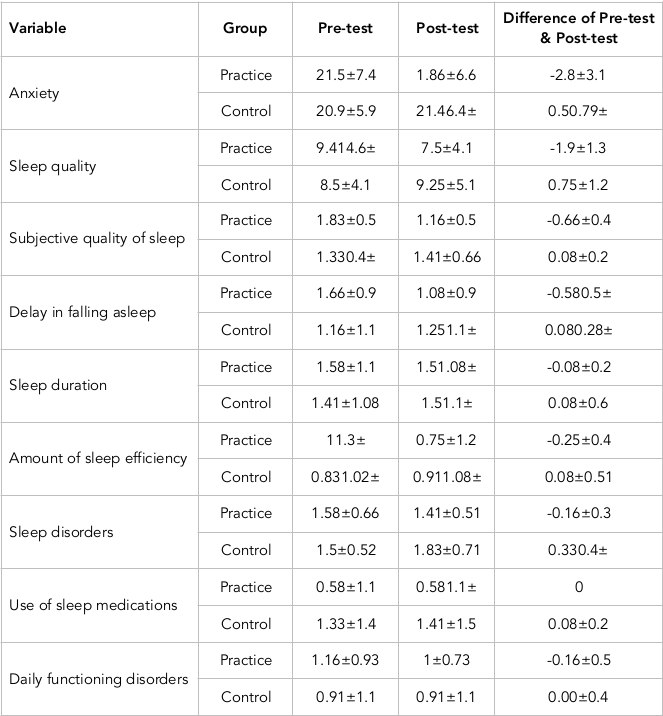
The Table 1 shows the mean and standard deviation of all variables in the pre-test evaluation, post-test evaluation, and the corresponding difference of pre-test and post-test values for the practice (experimental) and control groups.
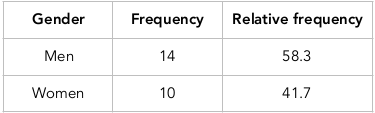
Table 2 shows the relative frequency of gender; it can be seen that 58.3% of the participants were men and 41.7% were women. The Mann-Whitney test results in Table 3 show that there is a significant difference between the average change in anxiety of patients suffering from Parkinson's disease in the laughter yoga practice (experimental) group (M=-2.83) versus the control group (M=0.50) (U=136, Z=3.76, P=0.000). Thus, the null hypothesis is rejected; in other words, a course of laughter yoga exercises led to a significant decrease of anxiety in patients suffering with Parkinson’s.
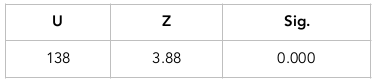
The Mann-Whitney test results depicted in Table 4 show that there is a significant difference between the average change in sleep quality of patients suffering from Parkinson's disease in the laughter yoga practice (experimental) group (M=-1.91) versus the control group (M=0.75) (U=138, Z=3.88, P=0.000). Thus, the null hypothesis rejected; in other words, a course of laughter yoga exercises led to a significant increase of sleep quality in patients with Parkinson's. Note that on the basis of scoring, the lower the sleep quality scores the better the sleep quality.
Discussion
The Mann-Whitney test results in Table 2 demonstrate that there is a significant difference between the average change in anxiety in patients with Parkinson’s in the laughter yoga practice (experimental) group versus the control group. In other words, the course of laughter yoga exercises led to a significant reduction in the anxiety of patients suffering from Parkinson's disease. According to the literature, these results are consistent with study results of Badr, 2014Bagheri, 2011Behzadi, 2010Bennett et al., 2003Eftekhari, 2004Hassed, 2001Hirosaki et al., 2013Keykhai Hosseinpour, 2013Kheirandish, 2014Moshfeghi, 2010Shahidi, 2008Sook and Hee, 2011. However, they differ from the study results of Omrani (2010).
As the results of our study are consistent with the aforementioned studies, it would seem that the predominant mechanism by which laughter influences anxiety is through its ability to establish and sustain a positive emotional state. During a state of anxiety, the adrenal gland frees corticosteroid hormones, which are converted to cortisol in the bloodstream. It is cortisol that increases in response to stress. Brouk (1998) believed that positive emotions such as laughter can reduce the ordinary stress response and as a moderator, amend sympathetic stimulation after stress Shahidi, 2008. Keykhai Hosseinpour (2013) conducted a research on the impact of laughter yoga exercises on the motor and mental factors of patients suffering from Parkinson’s Keykhai Hosseinpour, 2013. The results of his study indicated that laughter yoga exercises have a positive impact on reducing depression, thereby improving the patient’s quality of life and increasing motion performance, flexibility and pain reduction. His study concluded that Parkinson’s patients, as they have a lack of dopamine and serotonin, can use laughter yoga which help secrete hormones that help to reduce depression.
Depression and anxiety are among the most common mental problems of patients suffering from Parkinson’s. They arise due to the physical symptoms of the disease and also from the patient's disability. To combat this, laughter can be induced to provide benefits to the overall health status. Health benefits obtained of laughter yoga including physical, mental and emotional stress management.
When stress decreases, the immune system automatically becomes stronger. Laughter also increases the oxygen supply to cells of the body and increases blood circulation, thereby creating a positive state of health.
Given that the body can be influenced by a series of hormonal and physical changes which cause damage to the patient, any strategy that regularly reduces the level of stress hormones in the blood helps to increase health. Moreover, laughter is known to be a good stress inhibitor. In fact, joking and laughing can reduce the neuroendocrine hormones (epinephrine and cortisol) that are secreted in response to stress, causing the person to be calm Keykhai Hosseinpour, 2013. Laughter is one of the best, most cost-effective and easiest ways to relieve stress and relax the muscles of the body. Laughing dilates blood vessels and transmits more blood to the farthest muscles throughout the body. Furthermore, a good laugh from the heart reduces the secretion of stress hormones, epinephrine and cortisol.
When we are laughing there is no thought in our minds; all our senses seem to be synchronized for a brief moment. We feel joy, peace and comfort Behzadi, 2010. Also, according to the theory of emotional discharge, laughter is a socially acceptable way to release tension and stress. Provin (2000) argued that laughter in social interactions can be used as a stress relief mechanism. Spencer (according to the theory of drain excitement) believed that the emotional and mental turmoil produce a kind of energy that somehow must be used. He suggested that nervous excitement tended to cause muscle tension and that laughter, as a kind of physical movement, can act as a stream of various forms of nervous energy. Moreover, Spencer created the idea of laughter to remove bad potential energy through the process of daily stress management, constantly stacking energy and release of excess energy by laughing after a stressful day Provin, 2000.
Behzadi (2010) conducted a research study with the aim of evaluating the effectiveness of Katarya laughter therapy on increasing the general health of elderly residents in a nursing home of Shahid Hasheminejhad of Ray City Behzadi, 2010. The results of that research data showed that Katarya laughter therapy was significantly effective in increasing public safety, improving physical symptoms, anxiety and insomnia, increasing social dysfunctions, and reducing depression. According to the findings of that study, it was concluded that Katarya Laughter therapy can improve the health of residents in nursing homes. Thus, this treatment method (laughter) may be used as replacement or supplement for improving overall health of elderly in nursing home.
Hased (2001) reviewed numerous clinical studies which all demonstrated that humor and laughter can reduce stress in all situations. Laughter can affect inflammatory disorders, asthma, cancer, and heart disease. In his article, he identified several psychological impacts, including reduction of stress and anxiety, and improvement of mood, self-esteem and coping skills. In addition, Hased described a positive psychological effect on pain and an increase in the safety of certain factors, e.g. immunoglobulin A and white blood cells.
Omrani (2010) conducted a research study on the effect of music therapy and laughter therapy to reduce anxiety in women prior to surgery. That study was a quasi-experimental study with pre-test and post-test assessments. In Omrani’s study, the Katal anxiety test was used to measure stress; it was found that music therapy could reduce anxiety before surgery in women but that laughter did not have any therapeutic effect on anxiety of those women. In our study, however, laughter yoga exercises led to a significant increase in sleep quality of patients with Parkinson's disease (based on the scoring of the questionnaire on sleep quality). According to the literature, our study results are consistent with results of Badr, 2014Behzadi, 2010Fotouhi, 2010.
As mentioned in Introduction, the quality of sleep of those afflicted with Parkinson’s is influenced by factors such as anti-Parkinson's medications, Akintik pains, dystonia, restless legs syndrome, panic attacks, anxiety and depression, parasomnia, and sleep apnea. Laughter yoga is thought to impact all those factors, thereby improving sleep quality and ultimately alleviating the disorders.
Akintik pains usually occur due to lack of mobility in these patients and often lead to sleep disorders. Extreme rigidity, fever, pain in muscles and joints, headaches, and occasional pain in all parts of the body are all typical symptoms.
Laughter improves health by reportedly inducing the secretion of endorphins that reduce pain and promote the feeling of happiness Martin, 2001. In fact, laughing increases the level of endorphins, also considered to be natural painkillers. The secreted endorphins have been shown to help reduce pain in people suffering from arthritis, inflammation of the spine, and muscle spasms Kataria, 2004Pezeshki, 2012. Indeed, laughter is regarded as a pain management technique that can be used for most incurable diseases. People who are regularly practicing laughter therapy can secrete endorphins with a simple smile. A few minutes of real laughing can induce the equivalent results as rowing or stationary biking for 10-15 minutes Keykhai Hosseinpour, 2013. For the elderly who are not able to exercise, laughter is indeed a good secondary treatment option Keykhai Hosseinpour, 2013.
In addition to Akintik pains, other problems such as dystonia (i.e. involuntary muscle contractions of legs, fingers, wrists, ankles and feet) can cause painful cramps for Parkinson's patients Soleimani, 2015. In this regard, laughter yoga can improve muscles of the face, chest and abdomen. Indeed, muscle power is important and useful for hospitalized patients and elderly people who move around in a wheelchair. Kazines (1979) described laughter as running internal organs; that is, it is effective even for muscles of the digestive system and can help speed up the rate of digestion Keykhai Hosseinpour, 2013.
Another important advantage of laughter is decrease of muscle tension. Stress keep muscles in a contracted state. People who learn muscle relaxation methods can reach peace psychologically. In muscle relaxation methods, the therapist asks the patient firstly to perform of series of muscle contractions on his body muscles and then relax to feel the relaxation in those muscles. Laughter has been reported to decrease tension in the neck, shoulder and abdomen muscles Keykhai Hosseinpour, 2013. Joking and laughing reduce the hormones epinephrine and cortisol (which typically rise in response to stress), thereby leading to relaxation Keykhai Hosseinpour, 2013. As in the theory of emotional discharge, Freud believed that the release of energy is an enjoyable experience that is expressed as a laugh, thereby reducing tension and stress Shahidi, 2008.
Behzadi (2010) conducted a research with the aim of studying the effectiveness Katarya laughter therapy on the effect of general health of elderly residents of a nursing home in Hasheminejhad of Ray City Behzadi, 2010. Results of study showed that Katarya laughter therapy significantly increases public safety, improves physical symptoms, reduces anxiety and insomnia, and alleviates social dysfunction and depression. According to the findings of that study, it can be concluded that the method of Katarya laughter therapy is advantageous in removing negative thoughts, changing beliefs, creating positive emotional states, and reducing the symptoms of Parkinson’s disease. Overall, the general health of the senior home residents was markedly improved after laughter therapy.
Among other activities which affect the quality of sleep in patients with Parkinson's disease is respiratory disorder. One of the benefits of laughter yoga is, thus, improvement of the respiratory system. Laughter provides exercise to the lungs and chest muscles, resulting in improved vital capacity and breathing. In normal breathing when person is relaxed, there is a balance between inhalation and exhalation. In the stress and disease states, not only does breathing become more shallow and slower but the level of oxygen becomes lowered too. There is a great amount of air that remains in the lungs. By keeping the air in the lungs, oxygen content decreases and water vapor and carbon dioxide levels increase. In this case, the more favorable conditions for bacterial growth and lung infections are created.
Laughter increases ventilation and removes mucous plugs to help maintain air exchange which increases oxygen levels in the blood. In fact, when we laugh the air is completely expelled from the lungs and following that, carbon dioxide and water vapor is also emitted and replaced with oxygen. The oxygen becomes available to blood cells. The effects of laughter can benefit middle-aged people with chronic respiratory diseases, such as emphysema, and reduce the risk of infection and inflammation of the lungs Keykhai Hosseinpour, 2013. Therefore, laughter yoga can affect quality of sleep by improving the respiratory system.
Therefore, according to the benefits of laughter yoga, which include pain relief, muscle relaxation, reduced anxiety and depression, and improved respiratory system function, it can be concluded that laughter yoga does significantly improve sleep quality- either directly and indirectly- of patients with Parkinson's disease. The questionnaire (on sleep quality) by Peter Bourg evaluated 7 areas: sleep quality, sleep latency, sleep duration, sleep efficiency rate, sleep disturbances, use of sleeping pills, and daily functioning disorders.
Research limitations
All research studies have some limitations which are important to recognize and address for future insight. In this study, the limitations were as follows:
1. The number of individuals suffering from Parkinson’s, who are willing to cooperate in the study and participate in the laughter yoga exercises was very low; this was one of the greatest limitations of the study (contributing to a low sample size of experimental and control groups).
2. There was no possibility of taking advantage of the questionnaire for patients with Parkinson's disease due to the lack of standardized questionnaires in Iran. In the beginning, some steps were taken to standardize the questionnaires by translating it and having patients fill them out, but due to lack of time taking advantage of the questionnaire in this study was not feasible.
3. Due to the lack of accredited and essential facilities, there was no possibility of holding meetings in the hospital; all meetings were held at a house.
4. Due to general limitations for holding laughter yoga classes in the houses of the neighborhood, and despite initial agreement on the presence of the patient at the house and same time for holding the classes for women and men, it was decided that classes be held flexibly and separately, as needed.
5. Due to the age requirements, specific issues of some Parkinson’s patients and restrictions on the movements of these patients, not every patient could attend the regular meetings consistently.
Conclusion
In conclusion, laughter yoga significantly improves anxiety and sleep quality of Parkinson’s patients and can serve as a beneficial complementary therapy to standard therapy.
Author contribution
AZ performed data acquisition, data analysis; AS performed designed the study, data analysis and manuscript preparation; SMB performed data acquisition, and manuscript preparation. All authors approved the manuscript.
References
-
S.
Abargouei Azizi.
Effects of aquatic exercise therapy on quality of life, muscle strength and balance in patients with Parkinson's disease. In Faculty of Physical Education and Sports Sciences (Master's thesis).
2011
.
-
M.
Abedzadeh.
The effect of balance training on depression and quality of life of patients with Parkinson's disease. In Faculty of Physical Education and Sports Sciences (Isfahan University).
2012
.
-
M.
Afshar,
K.
Ghandehari.
Tremor in the right hand as the most common initial manifestation of Parkinson disease. Journal of Birjand University of Medical Sciences.
2006;
13
:
9-15
.
-
z.
Badr.
The effect of laughter therapy on general health and stress among nurses working in Yasuj hospitals. In Faculty of Humanities, Department of Psychology (Yasuj Branch: Islamic Azad University).
2014
.
-
r.
Bagheri.
The study of the effect of laughter therapy on group cataract on the reduction of occupational stress among female teachers of elementary school in District 13 of Tehran. In Faculty of Educational Sciences and Psychology (Allameh Tabatabaei University).
2011
.
-
A.
Behzadi.
The Effect of Kataria Laughter on Increased General Health in the Elderly Man in Shahid Hasheminejad Hospital. (Reyhaneh Charity and Charity Foundation) (Faculty of Educational Sciences and Psychology: Allameh Tabatabaei University).
2010
.
-
J.W.
Bellew,
J.W.
Yates,
D.R.
Gater.
The initial effects of low-volume strength training on balance in untrained older men and women. The Journal of Strength & Conditioning Research.
2003;
17
:
121-128
.
-
M.P.
Bennett,
J.M.
Zeller,
L.
Rosenberg,
J.
McCann.
The effect of mirthful laughter on stress and natural killer cell activity. Alternative therapies in health and medicine.
2003;
9
:
38
.
-
N.
Covassin,
A.B.
Neikrug,
L.
Liu,
J.
Corey-Bloom,
J.S.
Loredo,
B.W.
Palmer,
J.
Maglione,
S.
Ancoli-Israel.
Clinical correlates of periodic limb movements in sleep in Parkinson's disease. Journal of the neurological sciences.
2012;
316
:
131-136
.
-
L.E.
Dibble,
T.F.
Hale,
R.L.
Marcus,
J.
Droge,
J.P.
Gerber,
P.C.
LaStayo.
High-intensity resistance training amplifies muscle hypertrophy and functional gains in persons with Parkinson's disease. Movement Disorders.
2006;
21
:
1444-1452
.
-
S.
Eftekhari.
Comparison of the effectiveness of two methods of therapeutic play and laughter therapy on anxiety in children ages 6-12. In Islamic Azad University (Shahrood Branch: Faculty of Literature and Humanities).
2004
.
-
G.
Emsaki.
The cognitive functions of patients with Parkinson's disease compared with healthy subjects and the study of the effect of two drugs primaxyxol and thrigesifenidil on it. Iran: Isfahan University.
2010
.
-
M.
Fotouhi.
Determining the quality of sleep in patients referred to the Internal Clinic of the Neurology of Rasoul-Karm Hospital in the second half of 2010, undergoing deep brain stimulation. DBS (Tehran University of Medical Sciences and Health Services).
2010
.
-
M.L.
Giroux.
Parkinson disease: managing a complex, progressive disease at all stages. Cleveland Clinic journal of medicine.
2007;
74
:
313
.
-
A.O.
Hartmann,
WH.
Analysis of the motor disorder in Parkinson disease. In Parkinson disease: The treatment options, O.W. Lewitt PA, ed. (London: Martin Dunits).
2005;
:
39-50
.
-
H.
Hasan,
T.F.
Hasan.
Laugh yourself into a healthier person: a cross cultural analysis of the effects of varying levels of laughter on health. International journal of medical sciences.
2009;
6
:
200
.
-
C.
Hassed.
How humor helps keep you well. Australian Family Physician.
2001;
30
:
25-28
.
-
A.
Heydari,
P.
Ehteshamzadeh,
M.
Marashi.
The relationship between insomnia severity, sleep quality, sleepless and impaired mental health and academic performance of girls. Journal Woman Culture.
2010;
1
:
65-76
.
-
M.
Hirosaki,
T.
Ohira,
M.
Kajiura,
M.
Kiyama,
A.
Kitamura,
S.
Sato,
H.
Iso.
Effects of a laughter and exercise program on physiological and psychological health among community-dwelling elderly in Japan: Randomized controlled trial. Geriatrics & gerontology international.
2013;
13
:
152-160
.
-
Z.
Huang,
R.d.l.
Fuente-Fernández,
A.J.
Stoessl.
Etiology of Parkinson's Disease. Canadian Journal of Neurological Sciences / Journal Canadien des Sciences Neurologiques.
2014;
30
:
S10-S18
.
-
B.A.
Iranzo de RA,
V.
Campos.
Sleep disorders in Parkinson disease. Neurologist.
2011;
17
:
S38-S42
.
-
M.
Kataria.
Do not laugh at the reason! Translated by Majid Medical. Tehran: Nasle-no-Andish Publishing.
2004
.
-
A.
Keykhai Hosseinpour.
Laughter yoga exercises on psychomotor effects of Parkinson's patients. In Faculty of Physical Education and Sports Sciences (Isfahan University).
2013
.
-
A.
Kheirandish.
The Effect of Laugh Yoga on Stress and Depression in Multiple Sclerosis (MS) Patients. In Faculty of Psychology and Educational Sciences (Al-Zahra University).
2014
.
-
S.
Khorsand.
Laughter Yoga exercises influence on life satisfaction and depression among 65-70 year living in a nursing home. In the field of motor behavior. (The Islamic Azad University of Karaj).
2016
.
-
S.S.
Lord,
HB
C. Menz.
Falls in older people: risk factors and strategies for prevention. Cambridge: Cambridge University Press.
2003
.
-
R.
Margis,
K.
Donis,
S.V.
Schonwald,
S.C.
Fagondes,
T.
Monte,
P.
Martin-Martinez,
K.R.
Chaudhuri,
F.
Kapczinski,
C.R.
Rieder.
Psychometric properties of the Parkinson's Disease Sleep Scale--Brazilian version. Parkinsonism & related disorders.
2009;
15
:
495-499
.
-
R.A.
Martin.
Humor, laughter, and physical health: methodological issues and research findings. Psychological bulletin.
2001;
127
:
504
.
-
M.E.
Morris.
Movement disorders in people with Parkinson disease: a model for physical therapy. Physical therapy.
2000;
80
:
578-597
.
-
F.A.
Moshfeghi,
H.
Karim. Molawi Hussain. Chitsaz.
Efficacy of cognitive-behavioral group therapy for depression and quality of life in patients with Parkinson's disease in Isfahan. In Faculty of Education and Psychology (University of Isfahan).
2010
.
-
S.L.
Naismith,
I.B.
Hickie,
S.J.
Lewis.
The role of mild depression in sleep disturbance and quality of life in Parkinson's disease. The Journal of neuropsychiatry and clinical neurosciences.
2010;
22
:
384-389
.
-
M.R.
Najafi,
A.
Chitsaz,
Z.
Askarian.
Sleep Quality in Patients with Parkinson's Disease. Journal of Isfahan Medical School.
2012;
30
.
-
A.N.E.M.
Najarian,
Meysam. Hajj Fath Ali
Hamid. Mertazian.
The effect of heart rate variability levodopa in Parkinson's disease. 2008
.
-
A.J.
Nelson,
D.
Zwick,
S.
Brody,
C.
Doran,
L.
Pulver,
G.
Rooz,
M.
Sadownick,
R.
Nelson,
J.
Rothman.
The validity of the GaitRite and the Functional Ambulation Performance scoring system in the analysis of Parkinson gait\m {1}. NeuroRehabilitation.
2002;
17
:
255-262
.
-
M.
Pezeshki.
Power laugh. Now Andish Publisher.
2012
.
-
J.
Pierce.
Parkinson - Translation of Farhad Hemmatkhah. Peidayesh Publishing.
2008
.
-
R.
Provin.
Laughter. Penguin Books.
2000
.
-
K.
Robinson,
A.
Dennison,
D.
Roalf,
J.
Noorigian,
H.
Cianci,
L.
Bunting-Perry,
P.
Moberg,
G.
Kleiner-Fisman,
R.
Martine,
J.
Duda.
Falling risk factors in Parkinson's disease. NeuroRehabilitation.
2005;
20
:
169-182
.
-
D.
Scheller,
N.
Dürmüller,
P.
Moser,
R.D.
Porsolt.
Continuous stimulation of dopaminergic receptors by rotigotine does not interfere with the sleep-wake cycle in the rat. European journal of pharmacology.
2008;
584
:
111-117
.
-
M.
Shahidi.
Comparison of the efficacy of cataract funeral therapy and group exercise therapy in reducing depression and increasing the life satisfaction of elderly women living in Tehran. In Faculty of Psychology and Educational Sciences (Tehran: Allameh Tabatabaei University).
2008
.
-
K.
Shannon.
Movement disorders. In Neurology in clinical practice: principles of diagnosis and management, D.R. Bradley WG, Fenichel GM, ed. (Philadelphia: Butter worth-Heinemann).
2004;
:
2125-2169
.
-
A.W.M. H.
Shaumway cook.
Motor control: Teory and practical application. Baltimore MD: Williams & Willkins.
2007
.
-
M.A.
Soleimani,
Ameneh.
.Ya'qubzadeh.
Living with Parkinson. Tehran: Jamehenegar Publishing.
2015
.
-
S.H.
Sook,
R.K.
Hee.
Effects of Laughter Therapy on Postpartum Fatigue and Stress Responses of Postpartum Women. Journal of Korean Academy of Nursing.
2011;
41
.
-
M.E.
Tinetti.
Preventing falls in elderly persons. N Engl j Med.
2003;
2003
:
42-49
.
-
A.M.
Yektamaram.
Physical and motor rehabilitation of rehabilitation (Parkinson). Public relations office of the State Welfare Organization.
2010
.
-
B.t.
Yousefi,
J.
Vahid. Taherzadeh.
The effect of motion exercises therapy on quality of life in patients with Parkinson's disease. Olympic Journal.
2010;
72
.
Comments
Downloads
Article Details
Volume & Issue : Vol 4 No 07 (2017)
Page No.: 1463-1479
Published on: 2017-07-28
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 38330 times
- Download PDF downloaded - 8109 times
- View Article downloaded - 49 times
 Biomedpress
Biomedpress