Castleman's disease of the mesocolon: a rare case report
Abstract
Castleman’s disease is a rare form of localized lymph node hyperplasia of unknown etiology. The sub-types are; hyaline vascular, plasma cell and mixed variant. Clinical subtypes are localized (unicentric) and multicentric. It is reported in all age groups regardless of gender. Hyaline vascular type, accounts for 90% of all cases, often develops in the neck, mediastinum and pulmonary hilum. Its occurrence in the peritoneal cavity is very rare. We present a case in mesocolon of hyaline type in a 39 year female.
Introduction
Castleman’s disease (CD) is a rare form of localized lymph node hyperplasia of unknown etiology. The various histopathological sub-types are; hyaline vascular, plasma cell and mixed variant. Clinical subtypes are localized (unicentric) and multicentric Eszes et al., 2014. Most common type of unicentric CD is hyaline vascular type. Reported in all age groups regardless of gender Schaefer et al., 2011. It can occur in any part of the body as nodal/extranodal mass. Common sites are mediastinum (65%), Neck (16%), abdomen (12%) and axilla (3%) Guo et al., 2012. Its occurrence in the peritoneal cavity is very rare Miyoshi et al., 2013Papaziogas et al.,2006.
The definitive diagnosis of CD is based on histopathological examination. Hyaline vascular type is characterized by abnormal follicles with shrunken germinal centres consisting of follicular dendritic cells, ingrowing hyalinized blood vessels and the interfollicular hypervasularization Schaefer et al., 2011. Plasma cell variant shows hyperplastic germinal centres, intact mantle zone infiltrated by mature plasma cells and interfollicular plasmacytosis Schaefer et al., 2011. Mixed cellularity is a combination of hyaline vascular and plasma cell type. The hyaline vascular type most commonly presents as a single unicentric mass having a favourable prognosis, whereas the plasma cell type is almost always multicentric and harbours a worse prognosis Dei-Adomakoh et al., 2013.
Case Report
A 39 year old female presented with abdominal pain since 2 months. Pain was continuous, mild to moderate, and present in epigastric region. No history of altered bowel habits. General physical examination showed the patient was moderately built and well nourished. Laboratory investigations were within normal limits. Family history was insignificant. CT abdomen diagnosis was benign mesenchymal tumour/desmoid tumour/GIST. CT guided FNAC was done which revealed moderate cell yield consisting of benign spindle cells in cohesive sheets. A diagnosis of spindle cell tumour was given. Laprotomy was done, lesion was excised and sent for histopathological examination.
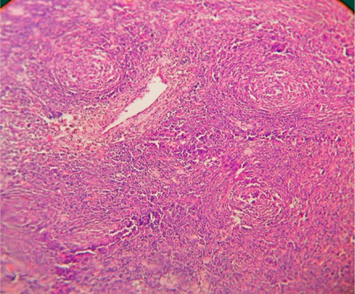
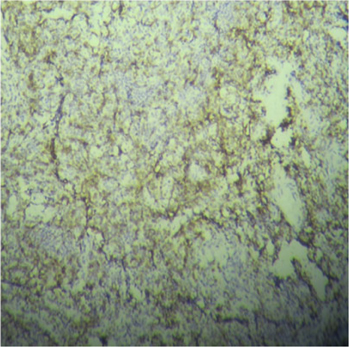
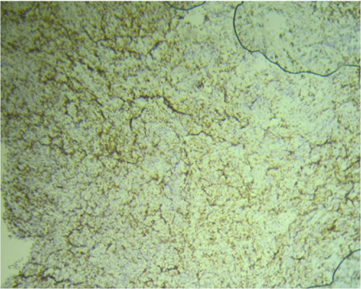
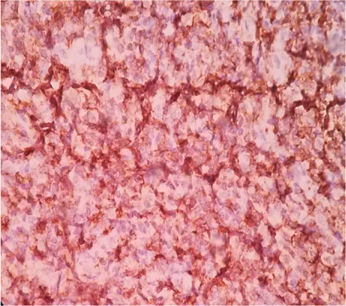
Grossly specimen was irregular, nodular, grey brown mass measuring 8x7x5cms ( Figure 1 ).Cut surface was gritty, grey white to grey brown with focal calcified areas. Microscopy showed structure of lymph node with effacement of normal architecture consisting of small lymphoid follicles with diminished germinal centre surrounded concentrically by mature lymphocytes. The centre of lymphoid follicles showed hyalinised blood vessels along with prominent dendritic cells ( Figure 2 , Figure 3 ). Focal areas showed prominent dilated sinusoids, marked fibrosis and calcification. Immunohistochemistry showed CD15, CD30 negative. CD45, CD20, CD3 and CD5 showed diffuse positivity ( Figure 4 , Figure 5 , Figure 6 , Figure 7 ). Finally diagnosis of Hyaline vascular type of Castleman’s disease (CD) was offered.
Discussion
Castleman’s disease is a rare form of localized lymph node hyperplasia of unknown etiology, also designated as angiofollicular lymph node hyperplasia, gaint lymphnode hyperplasia, angiomatous lymphoid hamartoma, benign giant lymphoma Ioachim H L, 2009. Studies have shown that CD is associated with increased production of cytokine interleukin-6 Tazi et al., 2011.
It was first described in 1954 by Benjamin castleman. Gaba et al described the first case along with histopathology in multiple lymph nodes in 1974 Fajgenbaum et al.,2014. Rachna M et al have reported that CD affects less than 2,00,000 people in the US population Madan et al., 2012. CD has been reported in all age groups regardless of gender. It can occur in any part of the body as nodal/extranodal mass with predilection for the mediastinum (65%), neck (16%), abdomen (12%) and axilla (3%). Its occurrence in the peritoneal cavity is very rare Miyoshi et al., 2013Papaziogas et al., 2006. The present case was in a 39 years female in the mesocolon.
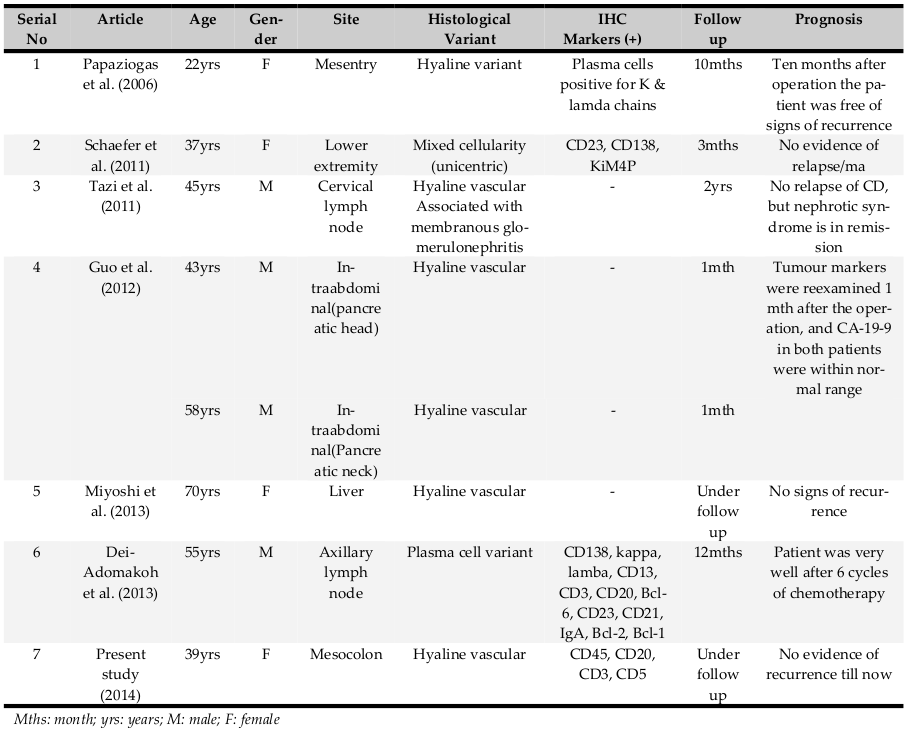
The clinical presentation depends on the clinical type; unicentric/multicentric. Unicentric CD is localized to particular region and is discovered incidentally or due to symptoms related to compression by the mass. Various studies have shown different locations which includes head and neck, intra-bronchial, intra-abdominal (pancreatic, liver, mesocolon), axillary lymph node, cervical lymph node and lower extremity Dei-Adomakoh et al., 2013Eszes et al., 2014Guo et al., 2012Miyoshi et al., 2013Papaziogas et al., 2006Schaefer et al., 2011Tazi et al., 2011. Table 1 shows the clinic- pathological characteristics of different subtypes of CD as described in the previous studies and the present case.
Most common histological type of unicentric CD is hyaline vascular type. On the other hand plasma cell type presents with signs of chronic inflammation such as fever, arthralgia, raised ESR and weight loss. Multicentric CD presents with multiple lesions and also in association with Kaposi sarcoma, autoimmune disorders and POEMS syndrome (peripheral oraganomegaly, endocrinopathy, monoclonal gammapathy (M-protein) and skin changes) Dei-Adomakoh et al., 2013. In present case the lesion was unicentric and histologically hyaline vascular type.
The definitive diagnosis of CD is based on histopathological examination. The histopathological subtypes of CD are hyaline vascular, plasma cell and mixed variant. On microscopic examination the hyaline vascular type is characterized by lymphoid follicles with shrunken germinal centres consisting of follicular dendritic cells, ingrowing hyalinized blood vessels and the interfollicular hypervasularization Schaefer et al.,2011.
Plasma cell variant shows hyperplastic germinal centers, intact mantle zone infiltrated by mature plasma cells and interfollicular plasmacytosis. Mixed cellularity is a combination of hyaline vascular and plasma cell type Schaefer et al., 2011. The present case was of hyaline vascular type.
The differential diagnoses of CD are other lymphoproliferative disorders especially lymphomas with plasmablastic features. HIV, HHV8 and EBV are associated with both plasmablastic lymphomas and CD. “B” cells are known to be characterized by CD5 expression in the expanded mantle zones of CD. CD shows positivity for CD45, CD20, CD3 and CD5 as in our case.
For localized unicentric variant, surgical resection of the affected lymph node is curative. Whereas MCD requires aggressive systemic therapy Dei-Adomakoh et al.,2013. The hyaline vascular type most commonly presents a single unicentric mass having a favourable prognosis, whereas the plasma cell type is almost always multicentric and has a worse prognosis. The present case was followed for one year which was uneventful.
Conclusion
To conclude, one should be aware of CD, its clinical/ histological types, prognosis for its early diagnosis and timely treatment.
Abbreviations
CD: Castleman’s disease
FNAC: Fine needle aspiration cytology
CT: Computerised tomography
GIST: Gastrointestinal stromal tumour
ESR: Erythrocyte sedimentation rate
MCD: Multicentric Castleman’s disease
Authors’ contributions
Mythri MB – Data collection, writing script. photography. Kalyani R – concept, data collection, revision of manuscript, editing manuscript, selecting gross and microphotograph images. Srinivas Murthy V – editing the manuscript.
References
-
Y.A.
Dei-Adomakoh,
C.
Segbefia,
I.
Ekem,
A.
Taylor.
Multicentric Castleman’s disease in a Ghanaian adult. Ghana medical journal.
2013;
47
:
92-95
.
-
N.
Eszes,
L.
Tamasi,
A.
Csekeo,
J.
Csomor,
A.
Szepesi,
G.
Varga,
G.
Balazs,
G.
Losonczy,
V.
Muller.
Unicentric mixed variant Castleman disease associated with intrabronchial plasmacytoma. Diagnostic pathology.
2014;
9
:
64
.
-
D.C.
Fajgenbaum,
F.
van Rhee,
C.S.
Nabel.
HHV-8-negative, idiopathic multicentric Castleman disease: novel insights into biology, pathogenesis, and therapy. Blood.
2014;
123
:
2924-2933
.
-
H.
Guo,
Y.
Shen,
W.L.
Wang,
M.
Zhang,
H.
Li,
Y.S.
Wu,
S.
Yan,
X.
Xu,
J.
Wu,
S.S.
Zheng.
Castleman disease mimicked pancreatic carcinoma: report of two cases. World journal of surgical oncology.
2012;
10
:
154
.
-
M.L.
Ioachim H L.
Castleman lymphadenopathy. In Ioachims Lymphnode Pathology Fourth.
2009;
:
227
.
-
R.
Madan,
J.H.
Chen,
B.
Trotman-Dickenson,
F.
Jacobson,
A.
Hunsaker.
The spectrum of Castleman’s disease: mimics, radiologic pathologic correlation and role of imaging in patient management. European journal of radiology.
2012;
81
:
123-131
.
-
H.
Miyoshi,
S.
Mimura,
T.
Nomura,
J.
Tani,
A.
Morishita,
H.
Kobara,
H.
Mori,
H.
Yoneyama,
A.
Deguchi,
T.
Himoto.
A rare case of hyaline-type Castleman disease in the liver. World journal of hepatology.
2013;
5
:
404-408
.
-
B.
Papaziogas,
G.
Chatzimavroudis,
I.
Koutelidakis,
M.
Grigoriou,
K.
Atmatzidis.
A rare form of isolated mesenteric Castleman’s disease presenting as an abdominal mass (isolated mesenteric Castleman’s disease). Journal of gastrointestinal and liver diseases : JGLD.
2006;
15
:
171-174
.
-
I.M.
Schaefer,
H.
Gunnel,
S.
Schweyer,
M.
Korenkov.
Unicentric castleman’s disease located in the lower extremity: a case report. BMC cancer.
2011;
11
:
352
.
-
I.
Tazi,
M.
Rachid,
A.
Quessar,
S.
Benchekroun.
A rare association of Castleman’s disease and nephrotic syndrome. Saudi journal of kidney diseases and transplantation : an official publication of the Saudi Center for Organ. Transplantation. Saudi Arabia.
2011;
22
:
116-119
.
Comments
Downloads
Article Details
Volume & Issue : Vol 1 No 03 (2014)
Page No.: 93-97
Published on: 2014-07-24
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 7194 times
- Download PDF downloaded - 1743 times
- View Article downloaded - 4 times
 Biomedpress
Biomedpress