Abstract
Introduction: Missed abortion is one type of abortions in which the product of a pregnancy is dead and does not leave the cervix, despite a long period of time. Missed abortion requires urgent action due to serious maternal complications. The purpose of this study was to investigate and compare the effects of using misoprostol on the treatment of missed abortions by two different methods.
Methods: In this retrospective study, 100 women with missed abortions at the pregnancy age of 4-6 weeks, who had been referred to Fatemieh Hospital of Hamadan and were candidates for termination of pregnancy, were randomly allocated into two equal groups. In the first group, 600 ug of misoprostol was administered sublingually, and in the second group, 600 ug of misoprostol was given vaginally. The treatment was repeated for both groups at intervals of 6 hours (3 times). Then, the patients were assessed at the 3rd, 6th and 12th hours after treatment for onset of bleeding and success of treatment (as well as abortion, with sonography). Data were analyzed by SPSS software version 16 with 95% confidence interval.
Results: In this study, the percentage of complete abortion in women receiving vaginal and sublingual misoprostol was 90% and 96%, respectively (p>0.05). The mean (SD) of misoprostol use was 1164 (467.02) and 924 (367.87) ug, respectively (P=0.004). The mean (SD) time interval between the use of the first tablet and the incidence of bleeding in women receiving misoprostol by sublingual and vaginal methods were 5.64 (1.85) and 7.47 (2.72) hours, respectively. Also, the time until the complete abortion for those receiving the sublingual and vaginal method was 7.10 (1.90) and 9.38 (2.53) hours, respectively (P<0.001).
Conclusion: In women with a missed abortion, prescribing 600 ug of misoprostol by sublingual method caused a bleeding event of shorter duration than the vaginal method, and complete abortion was achieved with a higher success rate.
Introduction
Abortion is often used to describe the failure of pregnancy in the first trimester of pregnancy, although it has been used to describe the loss of pregnancy before the 20th week1. Abortions are common occurrences in pregnancy, being seen at least in 15% of clinically diagnosed pregnancies2. A successful pregnancy is dependent on the integration of complex genetic, hormonal, immunologic and cellular events, and must involve complete cooperation during the conception, implantation and evolution of the embryo. Early pregnancy can happen due to a number of embryonic and embryonic factors. Most individual abortions occur due to intrinsic defects in pregnancy products, such as abnormal reproductive cells, incomplete implantation, deformities in the embryo, accidental injury to the embryo, and other possible causes previously unknown1.
Some factors such as anti-thyroid peroxidase antibody, non-insulin controls, insulin-dependent diabetes, and alcohol consumption are accompanied by an increase in the incidence of abortions. Immunologic factors, including anti-phospholipid antibody, are important factors in recurrent pregnancy loss. Some factors like hereditary thrombophilia, trauma, and cervical deficiencies are among other causes of abortion3. Since abortion and abortion control depends on numerous clinical factors, abortion has been monitored according to the following categories: threats to abortion, inevitable abortion, incomplete abortion, complete abortion, and recurrent abortions1. Missed miscarriage is an abortion in which a dead pregnancy product does not exit the uterus for a long period of time1. Abortion has a special importance due to serious maternal issues, such as bleeding disorders, shock, infection, rupture of uterus, and even mortality in women. Midwifery medicine and medical interventions are essential; common treatment involves medical and surgical interventions1,4.
The journey of a normal pregnancy for the women- without complications of maternal and fetal health- is an essential goal for the doctor. However, there are times when, even with the mother's tendency to continue pregnancy, the doctor will be forced to select an abortion5. Today, with the advancement of knowledge and new technologies, it is possible to make accurate diagnoses of abnormal pregnancies and to terminate a pregnancy in the early stages6. An abortion is an end to a pregnancy or surgery- before the embryo reaches the viability of survival- for embryonic or maternal reasons7. Traditionally, abortion has been done in the 1930s only by surgical procedures (dilatation and curettage), which are associated with high duty and mortality rates of 1% and 10 % morbidity, respectively, for the mother, including injuries, uterus injury, infections, and pregnancy remnants4,8. Both drug treatment and surgical drainage of the contents of the uterus have been tested and confirmed9. Surgery is a decisive and predictable method but it is aggressive and sometimes not necessary for all women3.
Today, the use of medications for treatment greatly increases the availability of safe and ineffective abortions, and has limited the use of surgical procedures10. Most of these methods use venous oxytocin at a high dose, prostaglandin (prescribed vaginally), and the E1 pill 11. In recent decades, medical abortion has been replaced by surgical methods. Several methods can be carried out in medical abortion, such as use of different drugs, including prostaglandins (misoprostol and dinoprostone), anti-progesterone, and antibiotics (methotrexate) 12. Studies with misoprostol have shown that this type of prostaglandin is a viable alternative for dilatation and curetage. Moreover, misoprostol can save patients from the risk of surgery and anesthesia13.
In recent years, misoprostol has been more widely used due to the impact of other methods and significant reductions of complication14. Misoprostol is a prostaglandin analog that has been confirmed to prevent and treat the stomach wound associated with non-steroidal anti-inflammatory drugs (NSAIDs)15. Misoprostol can soft the cervix and induce uterine contractions; therefore, it is used in induced abortion9. Misoprostol can be administered by the sublingual, vaginal, or rectal routes16. Several clinical trials have compared the outcome of prescribing different forms of misoprostol, but they have not gained convincing evidence in favor of one form over another.
A number of studies have suggested a positive and direct effect on the cervical/vaginal form17. Recent studies have shown the effectiveness of vaginal and vaginal method performance18. The purpose of this study was to investigate and compare the effects of using misoprostol on the treatment of missed abortion by two different methods (i.e. sublingual versus vaginal administration of misoprostol).
Methods
In this retrospective study, 100 women with forgotten abortions with a pregnancy age of 6-14 weeks, and who had been referred to Fatemieh Hospital of Hamadan from March 2016 to end of February 2018, were candidates for termination of pregnancy. Requests for Blood Group (BG), Rhesus factor (Rh), Complete Blood Count (CBC), liver tests, and kidney tests were randomly divided into two equal groups (based on the randomized block).
Sample size
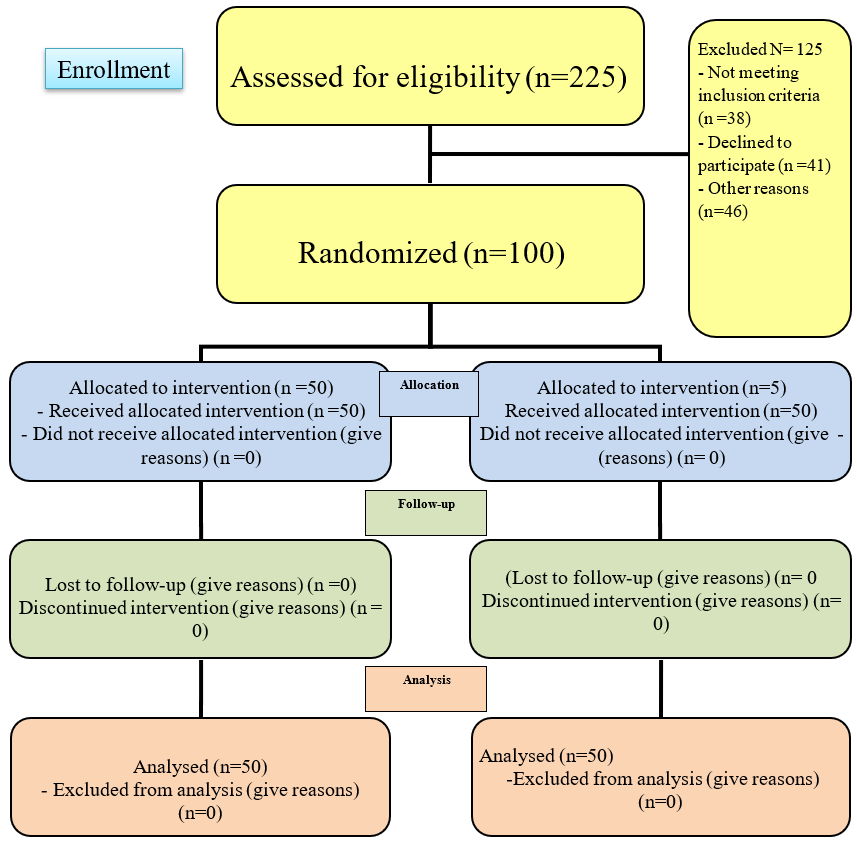
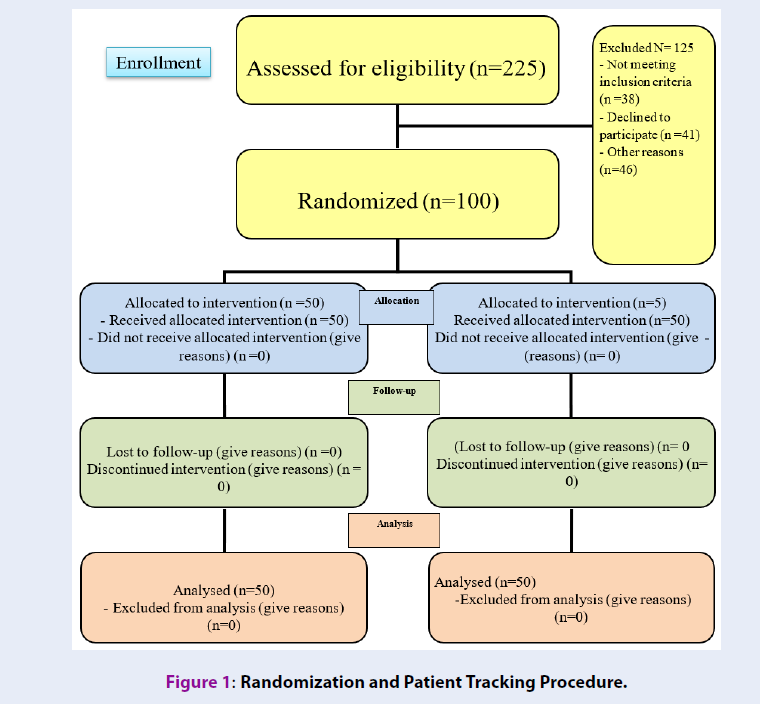
Several studies in this area can be conducted12,13,14,15, and the reported difference in the effects of these two methods was very close (difference in success rates were between 2 and 4% in most studies, 89% in the first group, and 93% in the second group. In one of the studies and using the results of this study, in the sample size estimation, the number of samples was very high (between 800 and 1000). Due to limitations of the research, in terms of the time period and access to this number of patients, it was deemed that the sample size was not feasible. Therefore, based on one of the valid studies that was similar to the present study13, the sample size was 100 people (Figure 1).
The inclusion criteria were: age of 6-14 weeks of pregnancy, not having cesarean section, having no systemic disease, the diagnosis of a specialized physician, and having the consent to participate in the study. Furthermore, the exclusion criteria included: severe hypersensitivity to misoprostol, uncontrolled seizures, and failure of the individual to track the outcome of treatment for any reason.
Instrumentation
For the data gathering tool in this study, a researcher-made checklist (including demographic characteristics of patients and the results of the intervention (including bleeding, abortion, and age of pregnancy). Furthermore, other components on the checklist include: having or not having cesarean section, group: vaginal or sublingual, initial dose of misoprostol tablets, and having or not having hemorrhage. In the event of bleeding, the time interval between tablet administration and bleeding/ hour (hr) can be related to abortion or no abortion. In the case of abortion, the duration of prescription prior to the abortion is noted, In case of non-abortions, the dosage of misoprostol (mcg) might affect abortion or might not. In the case of abortion, the duration (in hours) of the tablet until abortion is noted. In the case of non-abortions, the dose of misoprostol (µg) may affect abortion or may not. The interval (in hours) between the use of the first tablet and the incidence of bleeding is noted, as is the interval (in hours) between the use of the first tablet and the complete abortion.
In this study, all patients were enrolled in the study with written consent form. The checklist did not include the patients’ first or last names. This study was approved by the Committee on Ethics of the Vice-Chancellor of Research and Technology, Hamadan University of Medical Sciences (IR.UMSHA.REC.1395.35), with the Iranian Clinical Trials Code (IRCT) of IRCT201704179014N159.
Intervention
In the first group, patients received 600 µg of misoprostol tablets sublingually; in the second group, patients received 600 µg of misoprostol tablets vaginally. In both groups, the patients were examined for bleeding at 3, 6 and 12 hrs. If the bleeding did not start after 6 hours, the same dose of the drug was repeated. If abortion occurred at a given time interval, sonography was performed to assess the probability of the remaining pregnancy or an incomplete abortion. Success of the treatment was marked by the incidence of abortion after treatment and the absence of pregnancy abnormalities in the uterus (as confirmed by ultrasound).
Data analysis
Data were collected and analyzed by the SPSS software version 16. To describe quantitative data from mean and standard deviation, frequency and frequency were used to describe qualitative data. To analyze the nominal qualitative variables, the χ2 and independent quantitative variables were used. After determining the normality of the distribution of the data, T-student test was used, as well as the Mann-Whitney nonparametric test. The level of significance in this study was set at p <0.05.
| Complete Abortion | Group | p-value * | |
| Sublingual misoprostoln (%) | Vaginal misoprostolN (%) | ||
| Yes | 48(96) | 45(90) | 0.436 |
| No | 2(4) | 5(10) | |
| Total | 50(100) | 50(100) | |
| Treatment group | Mean | Standard deviation | P-value * |
| Sublingual misoprostol | 924 | 367.87 | 0.004 |
| Vaginal misoprostol | 1164 | 467.02 |
| Treatment group | Mean (±SD) | Minimum (hr) | Maximum (hr) | p-value * |
| Sublingual misoprostol | 5.64 (±1.85) | 3 | 12 | <0.001 |
| Vaginal misoprostol | 7.47 (±2.72) | 3 | 14 |
| Treatment group | Mean (±SD) | Minimum (hr) | Maximum (hr) | p. value * |
| Sublingual misoprostol | 7.10 (±1.90) | 3 | 4 | <0.001 |
| Vaginal misoprostol | 9.38(±2.53) | 3 | 6 |
Results
The findings of this study showed that the mean (±SD) of the gestational age in the vaginal and sublingual subgroups of the misoprostol group were: 10.86 (±2.83) and 10.85 (± 2. 52) weeks, respectively. There was no significant difference between the two groups regarding gestational age (P=0.361). The findings of this study showed that the percentage of abortion in women receiving vaginal and sublingual misoprostol was 90% and 96%, respectively. As a result, there was no significant difference between the two groups in the percentage of abortion (P=0.436) (Table 1). According to the results of this study, the mean dose of misoprostol in the vaginal administration (11364 μg) was significantly higher than that of the sublingual method (924 μg) (P=0.004) (Table 2).
The other finding of the present study showed that the mean interval between the use of the first tablet and the incidence of bleeding in the women receiving misoprostol by sublingual method was significantly lower than that of the vaginal method (P <0.001) (Table 3). In other words, the duration of bleeding in women who used the sublingual method was lower than that of women who used the vaginal method. According to the results of the above table, the mean interval between the use of the first pill and the incidence of complete abortion in women receiving sub-optimal misoprostol was significantly lower than that of women receiving the vaginal method (P <0.001) (Table 4). In other words, the duration of starting complete abortion in women who used the sublingual method was lower than that in women who used the vaginal method.
Discussion
The findings of this study showed that the mean (±SD) of the gestational age in the vaginal and sublingual subgroups of the misoprostol group were: 10.86 (±2.83) and 10.85 (±2.52) weeks, respectively. There was no significant difference between the two groups regarding gestational age (P=0.361). The findings of this study showed that the percentage of abortion in women receiving vaginal and sublingual misoprostol was 90% and 96%, respectively. As a result, there was no significant difference between the two groups in the percentage of abortion (P=0.436) (Table 1). According to the results of this study, the mean dose of misoprostol in the vaginal administration (11364 μg) was significantly higher than that of the sublingual method (924 μg) (P=0.004) Table 2).
The other finding of the present study showed that the mean interval between the use of the first tablet and the incidence of bleeding in the women receiving misoprostol by sublingual method was significantly lower than that of the vaginal method (P <0.001) (Table 3). In other words, the duration of bleeding in women who used the sublingual method was lower than that of women who used the vaginal method. According to the results of the above table, the mean interval between the use of the first pill and the incidence of complete abortion in women receiving suboptimal misoprostol was significantly lower than that of women receiving the vaginal method (P<0.001) (Table 4). In other words, the duration of starting complete abortion in women who used the sublingual method was lower than that in women who used the vaginal method.
Conclusions
In the sublingual method, the use of misoprostol leads to the induction of forgotten abortions; bleeding and abortions are significantly lower than the vaginal method in a shorter time period. The median dosage of the drug is lower than the vaginal method. Additionally, the success of misoprostol in abortion is somewhat greater than that of the vaginal method.
Abbreviations
Rh: Rhesus factor
BG: Blood Group
CBC: Complete Blood Count
Hr: Hour
μg: Micrograms
NSAID: Non-Steroidal Anti-Inflammatory Drug
Authors' Contributions
All authors contributed equally in the study design, interpretation of the data, and writing of the final manuscript.
Competing interests
The author(s) declare that they have no competing interests.
Acknowledgments
We thank the manager of Fatemieh hospital and also participants to participate in this study.
This study was supported by Hamadan University of Medical Sciences.
References
-
Kenneth
L.C.,
Gary
F.,
Williams Obstetrics & GynecologyMcGraw-Hill Education 2001.
Google Scholar -
Blohm
F.,
Fridén
B.,
Milsom
I.,
A prospective longitudinal population-based study of clinical miscarriage in an urban Swedish population. BJOG.
2008;
115
(2)
:
176-82
.
View Article PubMed Google Scholar -
Cunningham
F.,
Leveno
K.,
Bloom
S.,
Hauth
J.,
Gilstrap
L.,
Wenstrom
K.,
Prenatal diagnosis and fetal therapyWilliams Obstetrics 2010.
Google Scholar -
Rock
J.A.,
Jones
H.W.,
Te Linde's operative gynecologyLippincott Williams & Wilkins 2003.
Google Scholar -
Andrew
A. W.,
James
W. P.,
Sandra
H. B.,
Cindy
I.,
Stephen
S. E.,
.
Cause and effect analysis of closed claims in obstetrics and gynecology. Obstetrics & Gynecology.
2005;
105
(5)
:
1031-1038
.
-
Scott
R.S.,
Gibbs
B.Y.,
Karlan
A.F.,
Haney
A.,
Danforth's obstetrics and gynecologyLippincott Williams & Wilkins: Philadelphia; 2003.
Google Scholar -
Salari
Z.,
Sharifi
L.,
Comparison of the Efficacy of Vaginal Misoprostol with and without Laminaria in Second Trimester Induction Abortion. J Kerman Univ Med Sci.
2012;
19
(2)
.
-
Cunningham
F.G.,
Leveno
K.J.,
Bloom
S.L.,
Spong
C.Y.,
Dashe
J.S.,
Hoffman
B.L.,
Obstetrícia de WilliamsMcGraw Hill Brasil 2016.
Google Scholar -
Ngai
S.W.,
Tang
O.S.,
Ho
P.C.,
Prostaglandins for induction of second-trimester termination and intrauterine death. Best Pract Res Clin Obstet Gynaecol.
2003;
17
(5)
:
765-75
.
View Article PubMed Google Scholar -
WHO
Safe abortion: technical and policy guidance for health systemsWorld Health Organization 2003.
Google Scholar -
Pongsatha
S.,
Tongsong
T.,
Randomized controlled trial comparing efficacy between a vaginal misoprostol loading and non-loading dose regimen for second-trimester pregnancy termination. J Obstet Gynaecol Res.
2014;
40
(1)
:
155-60
.
View Article PubMed Google Scholar -
Speroff
L.,
Fritz
M.A.,
The clinical gynecologic endocrinology and infertility Lippincott Williams & Wilkins, Philadelphia 2005.
Google Scholar -
Beucher
G.,
Baume
S.,
Bekkari
Y.,
Legrand-Horras
M.,
Herlicoviez
M.,
Dreyfus
M.,
[Medical treatment of early spontaneous miscarriages: a prospective study of outpatient management using misoprostol]. J Gynecol Obstet Biol Reprod (Paris).
2004;
33
(5)
:
401-6
.
View Article PubMed Google Scholar -
Shaw
K.A.,
Topp
N.J.,
Shaw
J.G.,
Blumenthal
P.D.,
Mifepristone-misoprostol dosing interval and effect on induction abortion times: a systematic review. Obstet Gynecol.
2013;
121
(6)
:
1335-47
.
View Article PubMed Google Scholar -
Reilly
C.,
Wickersham
R.,
Schweain
S.,
Corrigan
C.,
Harms
K.,
Meekins
J.,
Drug facts and comparisonsWolters Kluwer Health: Missouri, St. Louis; 2006.
Google Scholar -
Tang
O.S.,
Lau
W.N.,
Ng
E.H.,
Lee
S.W.,
Ho
P.C.,
A prospective randomized study to compare the use of repeated doses of vaginal with sublingual misoprostol in the management of first trimester silent miscarriages. Hum Reprod.
2003;
18
(1)
:
176-81
.
View Article PubMed Google Scholar -
Tang
O.S.,
Lau
W.N.,
Chan
C.C.,
Ho
P.C.,
A prospective randomised comparison of sublingual and vaginal misoprostol in second trimester termination of pregnancy. BJOG.
2004;
111
(9)
:
1001-5
.
View Article PubMed Google Scholar -
Dickinson
J.E.,
Evans
S.F.,
A comparison of oral misoprostol with vaginal misoprostol administration in second-trimester pregnancy termination for fetal abnormality. Obstet Gynecol.
2003;
101
(6)
:
1294-9
.
PubMed Google Scholar
Comments
Downloads
Article Details
Volume & Issue : Vol 6 No 10 (2019)
Page No.: 3391-3395
Published on: 2019-10-23
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 20503 times
- View Article downloaded - 0 times
- Download PDF downloaded - 2041 times
 Biomedpress
Biomedpress