Abstract
Background: Arterial hypertension (AH) remains the most common cardiovascular (CV) risk factor worldwide.
Methods: Seventy five moderate-to-severe hypertensive patients with abdominal obesity aged from 48 to 66 years (45/30 men and women respectively) were selected from the entire cohort (n = 375) according to the inclusion and exclusion criteria. The patients were divided into two subgroups depending on the arm of antihypertensive therapy lines. The first subgroup of patients (n = 36) received a non-fixed combination of oral antihypertensive agents: perindopril (4–8 mg daily), indapamide (1.25–2.5 mg daily) and amlodopine (5–10 mg daily). The second subgroup of patients (n=39) received fixed-dosed combination of these antihypertensive agents aforementioned in the ranged doses (4 mg/1.25mg/5 mg; 4 mg/1.25mg/10 mg; 8 mg/2.5 mg/5 mg; 8 mg/2.5mg/10 mg) in the same manner. The examinations of the clinical status, office, and ambulatory blood pressure values were carried out at baseline in 3 and 6 months after study entry.
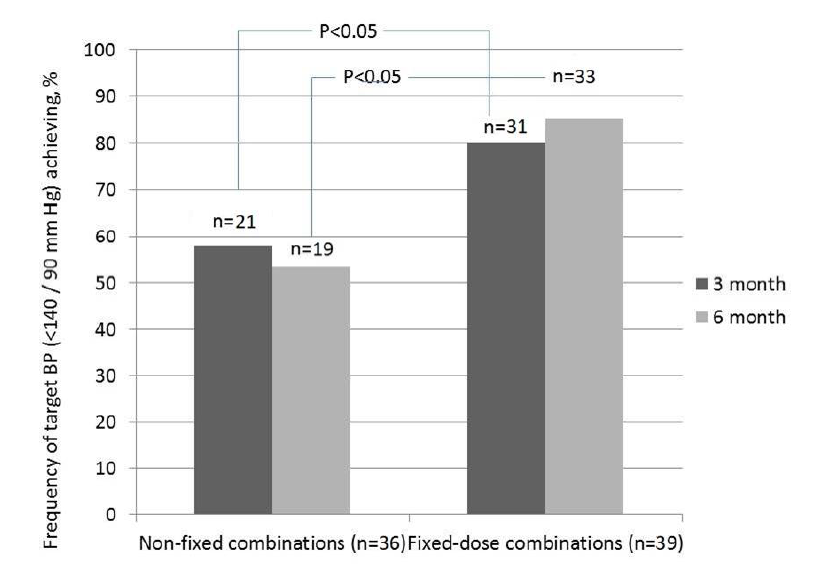
Results: The frequencies of BP target levels after treatment were higher in the fixed-dose combination group than in the non-fixed combination (at 3 months: 80% versus 58%, p<0.05 and at 6 months: 85% versus 53%, p<0.05). The adherence to triple fixed-dose combination was also higher in comparison with one to non-fixed combination (at 3 months: 82% versus 64%, p<0.05 and at 6 months: 87% versus 61%, p<0.05). It has been established that low-dose of perindopril/indapamide/amlodopine (4mg/1.25/10mg and 8mg/2.5/5mg) were used frequently in fixed-dose combination cohort of patients than in non-fixed combination (15% versus 0%, P<0.05, and 33% versus 19%, p<0.05, respectively). At the same time, maximum doses of these agents (8mg/2.5mg/10mg) were required for achieving target BP levels in a significantly lower proportion of patients receiving fixed-dose combination as compared to patients receiving non-fixed combination (52% versus 81%, p<0.05). Additionally, the triple fixed-dose combination has proved to be better in restoring ambulatory blood pressure monitoring profile than non-fixed combination.
Conclusion: Achievement of target blood pressure levels in patients with uncontrolled arterial hypertension and abdominal obesity was possible at lower doses of perindopril, indapamide, and amlodipine when used as a fixed-dose combination rather than non-fixed (free) combination.
Introduction
Arterial hypertension (AH) is the most common cardiovascular (CV) risk factor worldwide1,2. Prevalence of AH in European countries fluctuates from 20% to 50% of the adult population3,4. AH is frequently associated with various metabolic diseases including abdominal obesity (AO)5,6. In fact, at least 60% of AO patients were reported having mild-to-moderate AH7 and 15-20% of them had severe–to-refractory AH8. Moreover, endothelial dysfunction, dyslipidaemia, insulin resistance (IR), increased serum uric acid (SUA) - hypeuricemia (HUE), microvascular inflammation, which are accompanied to both AH and AO, can accelerate atherosclerosis, mediate pro-coagulation state and sufficiently elevate a risk of CV complications9,10,11. In this context, tight control for systolic and diastolic blood pressures (BP) at target levels (generally <140/90 mm Hg) is considered a useful tool for improving survival and preventing life-threatening events12,13. Unfortunately, double and triple combined anti-hypertensive therapy did not correspond to achieve target level of BP in many cases in patients with AO14. Previous studies have shown that more than half of patients needed double therapies to achieve full control in BP, while 20–30% of patients required triple combination and ever more15,16,17. It has been postulated that poor adherence to antihypertensive treatment, respectively high frequency of adverse effects and low tolerability could be the main causes to withdraw from the therapy18. Early prescription of triple fixed-dose combination could improve patient response to the treatment and consequently decrease CV risk. Substantiated triple fixed-dose combinations of angiotensin-converting enzyme (ACE) inhibitor perindopril (P), thiazide-like diuretic (TLD) indapamide (Ind), and long-acting dihydropyridine calcium channel blocker (CCB) amlodipine (Aml) is considered most promising to achieve high efficacy and superiority in safety when compared with the same non-fix dose combination19. The study aimed to investigate the efficacy of triple fixed-dose versus the non-fixed combination of P + Ind + Aml in obese patients with moderate-to-severe AH.
Methods
Seventy-five moderate-to-severe hypertensive patients with AO aged from 48 to 66 years (45 men and 30 women) were selected from the entire cohort (n=375) according to the inclusion and exclusion criteria (Figure 1). Inclusion criteria were patients with uncontrolled hypertension (systolic and/or diastolic BP levels > 140/90 mm Hg despite previous anti-hypertensive treatment with double drugs combination) at the study entry, age > 18 years and with written informed consent to participation in the study. Non-inclusion criteria includes patients with an acute coronary syndrome, acute myocardial infarction, heart failure, type 2 diabetes mellitus, angina pectoris, severe chronic renal failure, acute and chronic inflammatory diseases, severe liver insufficiency, chronic obstructive pulmonary disease, bronchial asthma, pregnancy, malignancy, and disability to know the reason of informed consent.
Study Design
This is an open-label, randomized, parallel-group and controlled study.
After the initial examination, the patients were divided into two subgroups depending on the arm of anti-hypertensive therapy lines. The first subgroup of patients (n=36) received a non-fixed combination of -anti-hypertensive agents, which include ACE inhibitor P (4–8 mg daily orally), TLD Ind (1.25–2.5 mg daily orally) and dihidroperidine CCB Aml (5–10 mg daily orally) non-fasting in the morning. The second subgroup of patients (n=39) received fixed-dosed combination of these anti-hypertensive agents mentioned above in the ranged doses (4 mg/1.25mg/5 mg; 4 mg/1.25mg/10 mg; 8 mg/2.5 mg/5 mg; 8 mg/2.5mg/10 mg) in the same manner. The examinations of the clinical status, office BP value was carried out at baseline, and in 3 and 6 months after the study entry, and ambulatory BP value was carried out at baseline and at 6 months after treatment. For target, BP levels systolic and diastolic BP <140/90 mm Hg were taken. All patients received recommendations about life-style modifications, and they were treated with atorvastatin 20 mg daily as a concomitant medication due to high-to very high CV risk.
Ethical declaration
The study was approved by the local Ethical Committee (Government Institution “L.T. Malaya Therapy National Institute of the National Academy of Medical Science of Ukraine," date of approval was 18.01.2018). All patients have given their voluntary informed consent to participate in the study.
Determination of AH
AH was diagnosed if systolic blood pressure (SBP) was >140 mm Hg, and/or diastolic blood pressure (DBP) >90 mm Hg, according to European guideline on diagnostics and treatment of arterial hypertension (2018)5, or a self-reported history of hypertension, and/or the use of anti-hypertensive medications.
Determination of risk factors and comorbidities
Determination of dyslipidemia
Dyslipidemia was diagnosed if total cholesterol (TC) level was above 5.2 mmol/L, and/or low density lipoproteid cholesterol (LDL) level was above 3.0 mmol/L, and/or triglyceride (ТG) level was above 1.7 mmol/L according to with European Cardiology Society dyslipidemia guideline (2016)20, or use of lipid-lowering medication.
Determination of AO
AO was defined as a body mass index (BMI) ≥30 kg/m2, waist circumference ≥90 cm in men or ≥80 cm in women21.
Determination of metabolic syndrome(MetS)
MetS was diagnosed based on the National Cholesterol Education Program Adult Treatment Panel III criteria22. Patients were enrolled in the MetS cohort when at least three of the following components were defined: waist circumference ≥90 cm in men or ≥80 cm in women; high density lipoprotein (HDL) cholesterol <1.03 mmol/L in men or <1.3 mmol/L in women; triglyceride levels ≥1.7 mmol/L; blood pressure ≥130/85 mmHg or current exposure of antihypertensive drugs; fasting plasma glucose ≥5.6 mmol/L.
Determination of HUE
HUE was diagnosed when blood serum levels of uric acid were found to be higher than 360 μmol/L.
Determination of family history of coronary artery disease (CAD)
A family history of CAD was defined if a first degree relative of any age was diagnosed with CAD, as mentioned in the self-report questionnaire.
Smoking status
Current smoking was defined as consumption of one cigarette daily for three months23.
Anthropometric measurements
Anthropometric measurements (weight, height, body mass, body mass index [BMI], waist circumference, and waist-to-hip ratio) were made using standard procedures24. Height and weight were measured by professional health staff, with the participants standing without shoes and heavy outer garments with a wall-mounted stadiometer (OMRON, Japan). BMI was calculated as weight (kg) divided by height squared (m2). Waist circumference was measured at the level midway between the lower rib margin and the iliac crest, with participants in a standing position without heavy outer garments, with emptied pockets and breathing out gently. Hip circumference was recorded as the maximum circumference over the buttocks.
Adherence to the treatment
Adherence to the treatment was measured as a percentage of the patients, who were not dropped out from the treatment arm due to several reasons including low tolerability, lowed compliance or lost for follow-up.
BP measure
Office BP was measured with the conventional method using a sphygmomanometer (Microlife BP AG 1-10, Hungary).
ECG recording
Standard 12-lead electrocardiography was performed at rest according to the conventional method with a three-channel FX-326U ECG recorder (Fukuda, Japan).
Ambulatory blood pressure monitoring (ABMP)
ABPM was performed according to contemporary protocol5 with AVRM-02/0 machine (Meditech, Hungary). Traditional parameters, such as SBP(24), average daily systolic BP; DBP(24), average daily diastolic BP; SBP(D), average daytime systolic BP; DBP(D), average daytime diastolic BP; SBP(N), average night-time systolic BP; DBP(N), average night-time diastolic BP; TISBP(24), time-index 24-hour SBP TIDBP(24), time-index 24-hour DBP; DNSBPR, degree of night-time SBP reduction; DNDBPR, degree of night-time DBP reduction; SBPV(24), average daily SBP variability; DBPV(24) and average daily DBP variability, were calculated and interpreted.
Echocardiography
Echocardiography was conducted in M- and B-modes with a 2.5 MHz phased probe using a medical diagnostic ultrasound complex SSD 280 LS (Aloka, Japan). The left ventricular myocardial mass (LVMM) and the LVMM index (LVMMI) were calculated by the formula of the American Society of Echocardiography. Left ventricular hypertrophy (LVH) was diagnosed when LVMMI increased to more than 50 g/m2 in men and 47 g/m2 for women5.
B-mode vascular ultrasound
B-mode common carotid artery (CCA) ultrasound examination was performed with a 7.5 MHz linear array probe using colour flow mapping by ultrasound scanner (LOGIQ-5, Japan). Thickness of intima-media segment (IMT) was measured according to conventional method25 Carotid IMТ values ≤ 0.9 mm were considered to be normal, IMТ was registered when its value was more than 0.9 mm, atheromatous plaques were registered when IMT value was >1.5 mm, or when carotid artery was locally thickened by 0.5 mm, or when IMT segment was up to 50% thicker than surrounding segments5.
Calculation of glomerular filtration rate (GFR)
GFR was calculated using CKD-EPI formula26.
Blood sampling
Blood samples were drawn immediately before study entry and at 6 months of investigation. Blood samples were centrifuged, serum was isolated within 30 min of sample acquisition and then freezed at -700C and stored in plastic tubes until being shipped to the laboratory of immune-chemical and molecular-genetic researches of Government Institution “L.T. Malaya Therapy National Institute of the National Academy of Medical Science of Ukraine".
Biomarker assay
The levels of plasma glucose, serum urea, creatinine, and uric acid were determined by enzymatic method using Humareazer 2000 analyzer (HUMAN GmbH, Germany).
Total cholesterol (TC), low density lipoprotein (LDL) cholesterol, high density lipoprotein (HDL) cholesterol, and triglyceride levels (TG) were measured by direct method on Humareazer 2106 analyser (HUMAN GmbH, Germany).
Hemoglobin A1c (HbA1c) were determined by high-pressure liquid chromatography method.
Fasting insulin level was measured by double-antibody sandwich immunoassay using commercial kits produced by DRG (Germany).
IR was assessed by the homeostasis model assessment for insulin resistance (HOMA-IR)27 using the following formula:
HOMA-IR (mmol/L × µU/mL) = fasting glucose (mmol/L) × fasting insulin (µU/mL) / 22.5.
IR was arbitrarily defined as HOMA-IR value above the 75th percentile of normal glucose tolerance, equal 2.45 mmol/L × µU/mL.
Statistics
Statistical analysis of the obtained results was performed in the SPSS system for Windows, Version 22 (SPSS Inc, Chicago, IL, USA). The data were presented as mean (М) and standard deviation (±SD) or 95% confidence interval (CI). To compare the main parameters of patient cohorts, a two-tailed Student t-test or Mann-Whitney U-test were used. To compare categorical variables between cohorts, the Chi2 test (χ2) and Fisher F exact test were performed. The three consequent comparisons for variables between each other and baseline were analysed using post-hoc ANOVA method with the Duncan test. A two-tailed probability value of <0.05 was considered as significant.
| Parameters | Entire group (n=75) | First cohort (n=36) | Second cohort (n=39) | р value |
|---|---|---|---|---|
| Age, years | 55.9±13.8 | 53.6±13.3 | 59.4±14.1 | NS |
| Male, n (%) | 45 (60%) | 22 (61%) | 23 (59%) | NS |
| Female, n (%) | 30 (40%) | 14 (39%) | 16 (41%) | NS |
| Moderate arterial hypertension (2nd stage of arterial hypertension), n (%) | 37 (49%) | 18 (50%) | 19 (49%) | NS |
| Severe arterial hypertension (3rd stage of arterial hypertension), n (%) | 38 (51%) | 18 (50%) | 20 (51%) | NS |
| Abdominal obesity stage 1, n (%) | 50 (67%) | 23 (64%) | 27 (69%) | NS |
| Abdominal obesity stage 2, n (%) | 25 (33%) | 13 (36%) | 12 (31%) | NS |
| Dyslipidaemia, n (%) | 67 (89%) | 32 (89%) | 35 (90%) | NS |
| Metabolic syndrome, n (%) | 72 (96%) | 34 (94%) | 38 (97%) | NS |
| LV hypertrophy, n (%) | 57 (76%) | 27 (75%) | 30 (77%) | NS |
| Carotid IMT >0.9 mm, n (%) | 40 (53%) | 18 (50%) | 22 (57%) | NS |
| LV mass index, g/m2 (male) | 60.6±11.3 | 57.2±11.7 | 63.8±10.9 | NS |
| LV mass index, g/m2 (female) | 54.5±11.3 | 53.2±11.7 | 56.8±10.9 | NS |
| Fasting glucose, mmol/L | 5.1±1.3 | 5.0±1.4 | 5.2±1.5 | NS |
| Creatinine, μmol/L | 90.4±21.1 | 92.1±19.6 | 89.3±22.4 | NS |
| SUA, μmol/L | 316.6±87.5 | 307.9±82.3 | 326.6±89.1 | NS |
| HOMA-IR, unit | 2.98±0.6 | 2.86±0.55 | 3.16±0.64 | NS |
| GFR, ml/min/1.73 m2 | 76.7±18.7 | 79.2±19.3 | 73.5±17.6 | NS |
| Total cholesterol, mmol/L | 5.92±1.21 | 5.57±1.17 | 6.14±1.23 | NS |
| LDL cholesterol, mmol/L | 3.97±0.82 | 3.66±0.79 | 4.24±0.83 | NS |
| HDL cholesterol, mmol/L (male) | 0.85±0.27 | 0.96±0.26 | 0.73±0.28 | NS |
| HDL cholesterol, mmol/L (female) | 1.12±0.27 | 1.15±0.26 | 1.03±0.28 | NS |
| Triglycerides, mmol/L | 2.33±0.38 | 2.18±0.37 | 2.54±0.41 | NS |
Results
The characteristics of the entire patient study population and both treatment arm cohorts are reported in Table 1. Among all groups of patients, moderate hypertension (2nd stage of hypertension) was found in 37 (49%) patients, severe hypertension (stage 3) — in 38 (51%), stage I AO found in 50 (67%) patients, stage II — in 25 (33%) patients. In the group of patients who were included in the study, a family history of hypertension was detected in 43 patients (78%). The following metabolic disorders were found: 67 (89%) patients with dyslipidaemia; 26 patients (35%) with fasting hyperglycemia (FHG), 53 (71%) patients with IR (HOMA-IR ≥2.77) and 20 (27%) patients with HUE.
Occurrence of asymptomatic hypertension-mediated organs damage among examined patients was as follows: pulse BP (PBP) increase (PBP≥60 mm Hg) was diagnosed in 29 (39%) patients, LVH - in 57 (76%) patients, carotid IMT >0.9 mm and/or atheromatous plaques - in 40 (53%) patients, and reduced to 45–59 ml/min/1.73 m2 GFR (stage IIIa chronic kidney disease (CKD) was found in 13 (170%) patients.
Figure 2 reports frequencies of BP target levels among all groups of patients. At 3 months and at 6 months of treatment, there were significant differences between numbers of patients in the groups having a target level of BP. Indeed, lower frequencies of BP target levels have appeared in patients treated with non-fixed triple combination in comparison with individuals taking triple fixed-does combination (р<0.05). However, 53% and 85% in moderate-to-severe hypertensive patients treated with non-fixed and fixed-does combination were found as those who have achieved BP<140/90 mm Hg after 6 months of treatment.
Additionally, 3-month and 6-month adherence to triple fixed-dose combination were higher (82% and 87%, respectively) in comparison with one to non-fixed combination (64% and 61%, respectively) (р<0.05) (Figure 3). While in the subgroup of patients treated with non-fixed combination of drugs adherence to therapy in 6 months tended to decrease compared to the rate of adherence in 3 months, in the group of patients who used fixed-dose combination of these drugs, adherence to treatment tended to increased with the continuation of treatment from 3 to 6 months from 82% to 87%.
| Non-fixed triple combination (n=36) | Fixed-dose triple combination (n=39) | р-value | |||
| n | % | n | % | ||
| Perindopril/indapamide/amlodipin: 4mg/1.25mg/10mg | 0 | 0 | 6 | 15 | =0.001 |
| Perindopril/indapamide/amlodipin: 8mg/2.5mg/5mg | 2 | 5 | 14 | 36 | =0.044 |
| Perindopril/indapamide/amlodipin: 8mg/2.5mg/10mg | 20 | 56 | 19 | 49 | NS |
| 8 mg Perindopril + 5 mg Amlodipin (free combination) | 6 | 17 | 0 | 0 | =0.012 |
| Took the medication irregularly | 5 | 14 | 0 | 0 | =0.01 |
| Didn’t take any medications | 3 | 8 | 0 | 0 | >0.05 |
For both cohorts, step-by step elevation of doses among all compounds embedded onto fixed and non-fixed combinations was specified (Table 2). It has been established that low-dosed triple fixed combination (4mg/1.25/10mg and 8mg/2.5/5mg) were used frequently in the second cohort to the first cohort to achieve target blood pressure. Moreover, 39% of patients, who were transferred to non-fixed combination, did not adhere to the given recommendations, and took only two medications (perindopril 8 mg daily and amlodipine 5 mg daily), or took medications irregularly or did not take any.
| Non-fixed triple combination (n=21) | Fixed-dose triple combination (n=33) | р value | |||
| n | % | n | % | ||
| Perindopril/indapamide/amlodipin: 4mg/1.25mg/10mg | 0 | 0 | 5 | 15 | =0.046 |
| Perindopril/indapamide/amlodipin: 8mg/2.5mg/5mg | 4 | 19 | 11 | 33 | =0.044 |
| Perindopril/indapamide/amlodipin: 8mg/2.5mg/10mg | 17 | 81 | 17 | 52 | =0.044 |
For individuals in the first and second cohorts with successful BP control, maximal doses of the agents (perindopril/indapamide/amlodipin: 8mg/2.5mg/10mg) were required in 81% and 52% respectively (р<0.05) (Table 3). Conversely, minimum and average doses of these agents were more commonly used by patients who were treated with fixed-dose combination, and reached target BP levels than by patients who were treated with non-fixed combination, and also reached target BP levels. It should be especially noted that 15% of patients with AH and AO treated with fixed-dose combination reached target BP levels after 6 months with minimum doses of these agents (perindopril/indapamide/amlodipin: 4mg/1.25/10mg). At the same time, such doses used in a non-fixed variation were not effective in patients to reach target levels of BP.
| Variables | Triple non-fixed combination (n=36) | Triple fixed-dose combination (n=39) | ||||
| Baseline | 6 month | Deviation from baseline | Baseline | 6 month | Deviation from baseline | |
| SBP(24), mm Hg | 151.31±10.67 | 136.35±11.09р<0.001 | -14.96±1.29 | 155.69±10.87 | 128.12±12.26 P<0.05 | -22.93±1.54 P1<0.05 |
| DBP(24), mm Hg | 92.50±12.75 | 84.69±10.95 | -6.8±2.95 | 94.79±10.49 | 77.93±10.99 р<0.001 | -15.86±1.12 р1<0.05 |
| SBP(D), mm Hg | 160.27±12.18 | 140.62±10.88 р<0.001 | -20.65±2.38 | 162.59±10.66 | 134.76±11.15 P<0.001 | -28.83±3.56 р1=0.05 |
| DBP(D), mm Hg | 94.23±10.46 | 86.23±11.85NS | -7.15±1.91 | 99.79±10.59 | 82.69±12.61р<0.001 | -16.86±3.32 р1=0.05 |
| SBP(N), mm Hg | 135.10±11.52 | 128.35±10.46 | -7.15±1.42 | 137.69±12.69 | 119.53±10.66р<0.001 | -17.86±1.78 р1<0.05 |
| DBP(N), mm Hg | 86.38±12.70 | 73.73±10.75 | -8.65±2.40 | 88.62±11.71 | 69.13±10.89 р<0.001 | -18.62±3.83 р1=0.05 |
| TISBP(24), % | 83.89±16.88 | 33.38±13.53 P<0.001 | -50.51±10.91 | 86.55±14.37 | 23.20±8.45 р<0.001 | -63.36±10.29 р1=0.05 |
| TIDBP(24), % | 62.65±12.91 | 31.27±9.59 Р=0.01 | -31.38±6.84 | 65.53±13.77 | 22.28±6.90 р<0.001 | -42.26±10.12 р1=0.05 |
| DNSBPR,% | 11.52±1.90 | 16.88±1.44р>0.05 | 5.37±1.06 | 9.16±1.64 | 18.34±1.35 р<0.001 | 9.19±1.75 р1=0.05 |
| DNDBPR,% | 8.45±1.59 | 11.78±1.38 р>0.05 | 3.33±0.74 | 7.66±0.22 | 15.47±1.59 р<0.001 | 8.81±0.56 р1=0.05 |
| SBPV(24), mm Hg | 17.54±1.44 | 12.62±1.22 NS | -4.92±0.74 | 20.10±1.35 | 9.34±0.92 р<0.001 | -10.34±1.43 р1=0.05 |
| DBPV(24), mm Hg | 15.62±1.36 | 10.42±1.21 р>0.05 | -5.19±0.36 | 17.55±1.37 | 8.31±0.92 р<0.01 | -8.24±0.45 р1=0.05 |
Ambulatory BP monitoring
6-month ABPM has shown that both triple non-fixed and triple fixed-dose combinations have driven a significant decrease in average daily systolic BP (SBP(24)), average daytime systolic BP (SBP(D)), time-index 24-hour SBP (TISBP(24)) and time-index 24-hour DBP (TIDBP(24)) (Table 4). However, the triple fixed-dose combination has been proved to be much better in restoring the ABPM profile. Additionally, triple fixed-dose combinations’ patients have exhibited significant decrease in average daily diastolic BP (DBP(24)), average daytime diastolic BP (DBP(D)), average night-time systolic BP (SBP(N)) and average night-time diastolic BP (DBP(N)). Patients also showed significant increase in a degree of night-time SBP reduction (DNSBPR) and degree of night-time DBP reduction (DNDBPR) and significant decrease in average daily SBP variability (SBPV(24)) and average daily DBP variability (DBPV(24)) (Table 4). Moreover, degrees of average daily systolic BP (SBP(24)), average daily diastolic BP (DBP(24)) and average night-time systolic BP (SBP(N)) reduction were sufficiently higher in triple fixed-dose combination patients compared to triple non-fixed combination individuals.
It was noted that there were no significant changes in SUA, serum uric and creatinine levels, estimating GFR, HOMA-IR, fasting glucose levels and BMI in both cohorts. Therefore, we did not find significant changes in LV mass index and carotid IMT for both cohorts.
Discussion
It was established that neither one of the patients received a fixed-dose combination of anti-hypertensive agents before inclusion in the study. The largest proportion of patients (80%) received two-component non-fixed combination of anti-hypertensive agents as a pre-study therapy. There was 47% of patients, who received combination of an ACE inhibitor or an angiotensin II receptor blocker (ARB) and a thiazide or thiazide-like diuretic, 24% of patients received combination of an ACE inhibitor or an ARB and a long-acting dihydropyridine CCB, and 9% of patients received combination of a beta-blocker and a thiazide-like diuretic. 20% of patients received a three-component combination of anti-hypertensive agents before inclusion in the study: ACE inhibitor or an ARB and a long-acting dihydropyridine CCB. However, 60% of these patients received treatment irregularly and not in sufficiently optimal daily doses. Both subgroups of patients who were transferred to non-fixed and fixed-dose combinations did not differ significantly by the types of the described pre-study therapy.
Consequently, transferring patients with uncontrolled AH and AO to non-fixed and fixed-dose three-component anti-hypertensive therapy with perindopril, indapamide and amlodipine significantly increased treatment efficacy. However, the use of a fixed-dose combination of these agents is significantly more effective than the use of the non-fixed combination.
One of the main reasons for achieving the higher and more stable effect of fixed-dose combination than non-fixed one was the better adherence to treatment in patients, who were treated with the fixed-dose combination of anti-hypertensive drugs16,19.
Of great clinical significance are the data obtained on complete normalization of the daily BP profile under the influence of the fixed-dose combination of perindopril, indapamide, and amlodipine, than that of under the influence of non-fixed combination5. It should be noted that the fixed-dose combination of these agents is useful in normalizing not only daily average and daytime average but also night-time average values of the daily BP profile.
An important result of this study was the absence of negative influence of the use of variants of non-fixed and fixed-dose combinations of perindopril, indapamide and amlodipine on metabolic parameters of patients with AH and AO5,15. The study showed that both non-fixed and fixed-dose combinations of these agents did not reduce efficacy of hypolipidemic therapy with average atorvastatin doses and contributed to significant decrease of dyslipidemia occurrence in patients with AH and AO. Moreover, it was found that when these patients were treated with the fixed-dose combination, their BMI occurrence values were significantly lower.
Both variants of combined therapy allowed slowing down the progression of cardiovascular and kidney diseases, inhibit the increase of LVH levels, stiffness and vascular wall remodeling (PBP elevation and carotid IMT and/or growth, or appearance of new atheromatous plaques in CCA), and slow down GFR reduction.
One of the most considerable results of the study was that lower doses of perindopril, indapamide and amlodipine are required for achieving target BP levels in patients with uncontrolled AH and AO if these agents are used as a fixed-dose combination.
It was found that maximum doses of perindopril, indapamide, and amlodipine were required for achieving target BP levels in a significantly lower proportion of patients receiving fixed-dose combination as compared to patients receiving a non-fixed combination of specified products.
Overall, it should be noted that combining agents of three anti-hypertensive drug groups, such as an ACE inhibitor, a TLD and a long-acting dihydropyridine CCB in one tablet contributes to significant increase of anti-hypertensive efficacy compared to non-fixed combination of these agents in patients with uncontrolled AH and AO4,15,18. An influential result of this study was also confirming better adherence of patients with hypertension and AO to fixed-dose combination of perindopril, indapamide, and amlodipine than to non-fixed combination of these agents. According to modern beliefs, better adherence to therapy is one of the most critical factors determining the possibility of achieving optimal control of hypertension in the population5,16.
Thus, this study has shown feasibility and perspectivity of a fixed-dose three-component combination of perindopril, indapamide and amlodipine use in patients with uncontrolled AH and AO. This is confirmed by findings of a number of published studies conducted in different groups of patients with AH and, most importantly, in patients with insufficiently controlled hypertension.
Study limitations
The main limitation of our study is the small number of patients. Because of this, it was not possible to perform subgroup analyses of the fixed-dose combination of perindopril, indapamide and amlodipine versus non-fixed combination within different subgroups (e.g., gender, age, hypertension, and obesity severity. Another potential limitation is that the post-baseline ABPM evaluation was done only at 6 months. Despite these limitations, the findings show the higher anti-hypertensive efficacy and more complete restoring of daily blood pressure profiles of the fixed-dose combination of perindopril, indapamide, and amlodipine in comparison with the non-fixed combination of these agents.
Conclusions
In conclusion, we found that the efficacy of the fixed-dose combination of perindopril, indapamide and amlodipine is significantly higher than non-fixed combination of these agents in patients with uncontrolled hypertension affected by AO. Using a fixed-dose combination of perindopril, indapamide and amlodipine in patients with uncontrolled hypertension and AO allow to significantly increase patients’ adherence to therapy by 26% compared to using the non-fixed combination. Patients with uncontrolled hypertension and AO receiving a fixed-dose combination of perindopril, indapamide, and amlodipine showed more complete normalization of the daily BP profile than patients receiving non-fixed combination. It was established that achievement of target BP levels in patients with uncontrolled AH and AO was possible at lower doses of perindopril, indapamide, and amlodipine when used as a fixed-dose combination rather than non-fixed (free) combination. Maximum doses of these agents were required for achieving target BP levels in a significantly lower proportion of patients, who received fixed-dose combination when compared to patients receiving a non-fixed combination of these products.
Abbreviations
ABPM: Ambulatory Blood Pressure MonitoringACE: angiotensin-converting enzymeAH: arterial hypertensionAml: amlodipineAO: abdominal obesityBMI: body mass indexBP: blood pressureCAD: coronary artery diseaseCCB: calcium channel blockerCI: confidence intervalCV: cardiovascularDBP: diastolic blood pressureDBP(N): average night-time diastolic blood pressureDBPV(24): average daily diastolic blood pressure variabilityDNDBPR: degree of night-time diastolic blood pressure reductionDNSBPR: degree of night-time systolic blood pressure reductionGFR: glomerular filtration rateHDL: high density lipoprotein cholesterolHOMA-IR: homeostasis model assessment for insulin resistanceHUA: hyperuricemiaIMT: carotid intima-media segment thicknessInd: indapamideIR: insulin resistanceLDL: low density lipoprotein cholesterolLVH: left ventricular hypertrophyLVMMI: left ventricular myocardial mass indexMetS: metabolic syndromeP: perindoprilSBP: systolic blood pressureSBP(N): average night-time systolic blood pressureSBPV(24): average daily systolic blood pressure variabilitySUA: serum uric acidTC: total cholesterolTG: triglyceridesTIDBP(24): time-index 24-hour diastolic blood pressureTISBP(24): time-index 24-hour systolic blood pressureTLD: thiazide-like diuretic
Competing Interests
Not declared.
Financial disclosure
There has been no significant financial support for this work that could have influenced its outcome.
Authors' Contributions
S.M. Koval initiated the hypothesis and designed the study protocol. I.O. Snihurska enrolled the patients; collected and analyzed the data reviewed the source documents. T.G. Starchenko and M.Y. Penkova contributed to enroll the patients in the study and collected the data. O.V. Mysnychenko and K.O. Yushko performed of blood collection and interpreted of the obtained results. O.M. Lytvynova and O.V. Vysotska contributed to collect, analyze and interpret the data, and performed statistical analysis. A.E. Berezin performed statistical analysis, wrote the manuscript and approved final version of the paper. All authors read the manuscript before submitting and agree with final version of the paper.
Statement of Originality
The authors do hereby declare that all materials used herein are original. This study is not under consideration for publication elsewhere. We confirm that the manuscript has been read and approved by all named authors and that there are no other persons who satisfied the criteria for authorship but are not listed. We further confirm that the order of authors listed in the manuscript has been approved by all of us. We understand that the Corresponding Author is the sole contact for the Editorial process (including Editorial Manager and direct communications with the office). He is responsible for communicating with the other authors about progress, submissions of revisions and final approval of proofs.
References
-
Sinnott
S.J.,
Smeeth
L.,
Williamson
E.,
Douglas
I.J.,
Trends for prevalence and incidence of resistant hypertension: population based cohort study in the UK 1995-2015. BMJ.
2017;
358
:
j3984
.
View Article PubMed Google Scholar -
Amiri
P.,
Vahedi-Notash
G.,
Naseri
P.,
Khalili
D.,
Hashemi Nazari
S.S.,
Mehrabi
Y.,
National trends of pre-hypertension and hypertension among Iranian adolescents across urban and rural areas (2007-2011). Biol Sex Differ.
2019;
10
(1)
:
15
.
View Article PubMed Google Scholar -
Achelrod
D.,
Wenzel
U.,
Frey
S.,
Systematic review and meta-analysis of the prevalence of resistant hypertension in treated hypertensive populations. Am J Hypertens.
2015;
28
(3)
:
355-61
.
View Article PubMed Google Scholar -
James
P.A.,
Oparil
S.,
Carter
B.L.,
Cushman
W.C.,
Dennison-Himmelfarb
C.,
Handler
J.,
2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA.
2014;
311
(5)
:
507-20
.
View Article PubMed Google Scholar -
Williams
B.,
Mancia
G.,
Spiering
W.,
Agabiti Rosei
E.,
Azizi
M.,
Burnier
M.,
Scientific Document Group
ESC,
2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J.
2018;
39
(33)
:
3021-104
.
View Article PubMed Google Scholar -
Falaschetti
E.,
Mindell
J.,
Knott
C.,
Poulter
N.,
Hypertension management in England: a serial cross-sectional study from 1994 to 2011. Lancet.
2014;
383
(9932)
:
1912-9
.
View Article PubMed Google Scholar -
Egan
B.M.,
Zhao
Y.,
Axon
R.N.,
Brzezinski
W.A.,
Ferdinand
K.C.,
Uncontrolled and apparent treatment resistant hypertension in the United States, 1988 to 2008. Circulation.
2011;
124
(9)
:
1046-58
.
View Article PubMed Google Scholar -
Armario
P.,
Calhoun
D.A.,
Oliveras
A.,
Blanch
P.,
Vinyoles
E.,
Banegas
J.R.,
Prevalence and Clinical Characteristics of Refractory Hypertension. J Am Heart Assoc.
2017;
6
(12)
:
e007365
.
View Article PubMed Google Scholar -
Orlando
A.,
Viazzi
F.,
Giussani
M.,
Nava
E.,
Cazzaniga
E.,
Bonino
B.,
Endothelin-1/nitric oxide balance and HOMA index in children with excess weight and hypertension: a pathophysiological model of hypertension. Hypertens Res.
2019;
42
(8)
:
1192-9
.
View Article PubMed Google Scholar -
De Becker
B.,
Borghi
C.,
Burnier
M.,
van de Borne
P.,
Uric acid and hypertension: a focused review and practical recommendations. J Hypertens.
2019;
37
(5)
:
878-83
.
View Article PubMed Google Scholar -
Koval
S.M.,
Snihurska
I.O.,
Vysotska
O.,
Strashnenko
H.M.,
Wójcik
W.,
Dassibekov
K.,
Prognosis of essential hypertension progression in patients with abdominal obesity.. 2019
.
View Article Google Scholar -
Kario
K.,
Thijs
L.,
Staessen
J.A.,
Blood Pressure Measurement and Treatment Decisions. Circ Res.
2019;
124
(7)
:
990-1008
.
View Article PubMed Google Scholar -
Gupta
A.K.,
Arshad
S.,
Poulter
N.R.,
Compliance, safety, and effectiveness of fixed-dose combinations of antihypertensive agents: a meta-analysis. Hypertension.
2010;
55
(2)
:
399-407
.
View Article PubMed Google Scholar -
Mancia
G.,
Rea
F.,
Corrao
G.,
Grassi
G.,
Two-Drug Combinations as First-Step Antihypertensive Treatment. Circ Res.
2019;
124
(7)
:
1113-23
.
View Article PubMed Google Scholar -
Ettehad
D.,
Emdin
C.A.,
Kiran
A.,
Anderson
S.G.,
Callender
T.,
Emberson
J.,
Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet.
2016;
387
(10022)
:
957-67
.
View Article PubMed Google Scholar -
Schroeder
K.,
Fahey
T.,
Ebrahim
S.,
How can we improve adherence to blood pressure-lowering medication in ambulatory care? Systematic review of randomized controlled trials. Arch Intern Med.
2004;
164
(7)
:
722-32
.
View Article PubMed Google Scholar -
Vysotska
O.V.,
Koval
S.M.,
Bespalov
Y.G.,
Pecherska
A.I.,
Lytvynova
O.M.,
Dyvak
A.M.,
Mathematical simulation of the structure of pulsed arterial pressure relations with vascular damage factors in patients with arterial hypertension.. 2019
.
View Article Google Scholar -
Walsh
J.M.,
McDonald
K.M.,
Shojania
K.G.,
Sundaram
V.,
Nayak
S.,
Lewis
R.,
Quality improvement strategies for hypertension management: a systematic review. Med Care.
2006;
44
(7)
:
646-57
.
View Article PubMed Google Scholar -
Glynn
L.G.,
Murphy
A.W.,
Smith
S.M.,
Schroeder
K.,
Fahey
T.,
Interventions used to improve control of blood pressure in patients with hypertension. Cochrane Database Syst Rev.
2010;
:
005182
.
View Article Google Scholar -
Catapano
A.L.,
Graham
I.,
De Backer
G.,
Wiklund
O.,
Chapman
M.J.,
Drexel
H.,
Authors/Task Force Members
2016 ESC/EAS Guidelines for the Management of Dyslipidaemias: The Task Force for the Management of Dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS) Developed with the special contribution of the European Assocciation for Cardiovascular Prevention & Rehabilitation (EACPR). Atherosclerosis.
2016;
253
:
281-344
.
View Article PubMed Google Scholar -
Alberti
K.G.,
Eckel
R.H.,
Grundy
S.M.,
Zimmet
P.Z.,
Cleeman
J.I.,
Donato
K.A.,
International Diabetes Federation Task Force on Epidemiology
Prevention
Hational Heart
Lung,
Blood Institute
American Heart Association
World Heart Federation
International Atherosclerosis Society
International Association for the Study of Obesity
Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation.
2009;
120
(16)
:
1640-5
.
View Article PubMed Google Scholar -
National Cholesterol Education Program (NCEP) Expert Panel on Detection
Evaluation,
Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III)
Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation.
2002;
106
(25)
:
3143-421
.
View Article PubMed Google Scholar -
Lindson-Hawley
N.,
Begh
R.,
McDermott
M.S.,
McEwen
A.,
Lycett
D.,
The importance of practitioner smoking status: a survey of NHS Stop Smoking Service practitioners. Patient Educ Couns.
2013;
93
(1)
:
139-45
.
View Article PubMed Google Scholar -
World Health Organization
World Health Organization: Geneva; 2008.
Google Scholar -
Gómez-Marcos
M.A.,
Recio-Rodríguez
J.I.,
Patino-Alonso
M.C.,
Agudo-Conde
C.,
Gómez-Sanchez
L.,
Gómez-Sanchez
M.,
Protocol for measuring carotid intima-media thickness that best correlates with cardiovascular risk and target organ damage. Am J Hypertens.
2012;
25
(9)
:
955-61
.
View Article PubMed Google Scholar -
Levey
A.S.,
Stevens
L.A.,
Schmid
C.H.,
Zhang
Y.L.,
Castro
A.F.,
Feldman
H.I.,
(Chronic Kidney Disease Epidemiology Collaboration)
CKD-EPI,
A new equation to estimate glomerular filtration rate. Ann Intern Med.
2009;
150
(9)
:
604-12
.
View Article PubMed Google Scholar -
Matthews
D.R.,
Hosker
J.P.,
Rudenski
A.S.,
Naylor
B.A.,
Treacher
D.F.,
Turner
R.C.,
Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia.
1985;
28
(7)
:
412-9
.
View Article PubMed Google Scholar
Comments
Downloads
Article Details
Volume & Issue : Vol 6 No 11 (2019)
Page No.: 3501-3512
Published on: 2019-11-30
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
- HTML viewed - 10275 times
- Download PDF downloaded - 2259 times
- View Article downloaded - 0 times
 Biomedpress
Biomedpress





