Abstract
Introduction: Placental teratoma is an uncommon, non-trophoblastic benign tumor. Since the first description of this type of tumor by Morvilli in 1925, only a few cases of this abnormality have been diagnosed and reported.
Case presentation: We describe here a 35-year-old pregnant woman admitted for an elective cesarean section. The placenta and membranes were delivered spontaneously. After delivering the placenta, a tumor mass containing hair was detected between the extraplacental amnion and chorion. On gross examination, a singleton placenta weighing 173 g, measuring 15 × 11 cm in area and 5.5 cm thick, with an attached cord and membranes, was observed. Microscopic examination showed orthokeratinized stratified squamous epithelium with underlying hair follicles, telangiectatic vessels, and sebaceous glands accompanied by subcutaneous fat. The fat also contained fibrocollagenous bundles. In addition, interconnecting bone trabecula rimmed by osteoblasts and attached mature cartilage were also found.
Conclusion: An awareness of placental teratoma from a pathological perspective is needed to include this anomaly in the differential diagnosis of benign placental nodules, obtain more information about this unusual lesion, and to conduct more studies on this prenatal abnormality.
Introduction
Teratomas are a type of germ cell tumor and can be divided into two types: mature and immature. These tumors contain multiple germ cell layers and are made up of several different types of tissue, such as hair, fat, and bone. The most common sites for these tumors are the ovary, testis, anterior mediastinum, posterior peritoneum, and pre-sacral region. Ovarian teratoma accounts for 15 to 20% of all ovarian tumors. Placental teratoma is considered to be a rare, non-trophoblastic benign tumor1, 2. Since the first description by Morvilli in 1925, only a few cases of placental teratoma have been diagnosed and reported3. In all cases identified, the teratoma was located between the amnion and chorion, usually on the fetal surface of the placenta. Placental teratomas are very similar to fetus amorphous, but the umbilical cord and skeletal central structure are not detected in the teratoma4, 5. In one case report, the teratoma was mistaken for an encephalocele6. Prenatal diagnosis of placental teratoma is important because most are benign and do not appear to increase the risk of congenital malformations or complications of a normal pregnancy1. However, a placental teratoma may present a diagnostic challenge. In this report, we describe a placental teratoma that did not lead to obstetrical complications. Only a few such cases have been reported globally, and none of them in Iran.
Case presentation
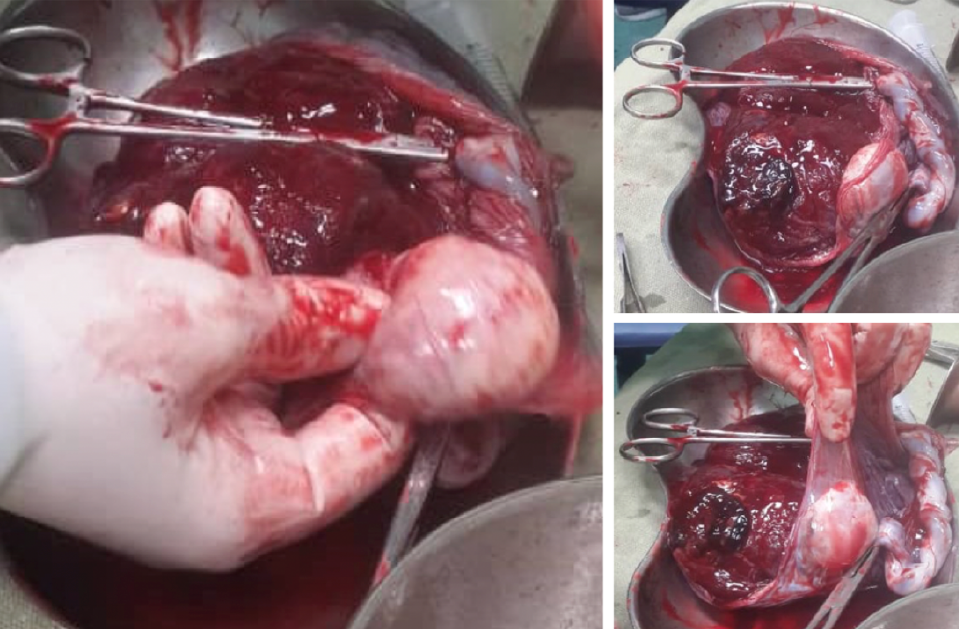
A 35-year-old pregnant woman with G4L2D2 (twin) REPIV, was admitted at 37 weeks +1 day for an elective cesarean section (post previa with focal accreta). Up to the 15th week of pregnancy, regular follow-up was carried out for gestational diabetes, which was controlled with diet. The patient’s previous delivery was by cesarean section. The patient’s blood group was B+, and she had a normal delivery of a female infant weighing 2500 g, with an Apgar score of 9/10. The placenta and membranes were delivered spontaneously. The placenta was previa but showed no focal accreta. After delivering the placenta, a tumor mass, containing hair, was found between the extraplacental amnion and the chorion (Figure 1). Although the patient had received antenatal care, the tumor was not identified antenatally by ultrasound. Sex chromatin and ploidy examination were not performed in this patient.
Upon gross examination, a singleton placenta weighing 173 g and measuring 15 × 11 cm in area and 5.5 cm in thickness, with an attached cord and membranes, was observed. The umbilical cord was inserted in an unusual manner and measured 15 cm in length and 1 cm in diameter. A cross-section of the cord revealed two vessels. The membranes were unremarkable and measured 23 × 16 cm in area and 1 cm in thickness. An excised section of the placenta showed no obvious lesions. A mass with a rubbery consistency measured 4 × 3.5 × 1.5 cm. A vessel through this mass was connected to the placenta at a peripheral aspect and a distance of 4 cm from the umbilical cord and was supplied by a vascular structure originating from the placenta.
Microscopic examination showed orthokeratinized stratified squamous epithelium with underlying hair follicles, telangiectatic vessels, and sebaceous glands accompanied by subcutaneous fat, which was transversed by fibrocollagenous bundles, as well as interconnecting bone trabecula rimmed by osteoblasts and attached mature cartilage (Figure 2).
Discussion
Tumors of the placenta are divided into trophoblastic and non-trophoblastic types, with the latter characterized as either primary or secondary. The most common type of non-trophoblastic and primary placental tumor is chorangioma, which occurs in 1% of all pregnancies7, 8. The second most common non-trophoblastic and primary placental tumor is a teratoma, first described in 1925 by P. Morvilli3. Placental teratomas are rare tumors with an unclear histogenesis5, 9. Nicholson proposed the “included twin” hypothesis, in which it was suggested that the teratoma initiated from a twin fetus that was “included” or merged with its co-twin through an embryological anomaly10. Tavares and Oporto speculated that the teratoma cell line arises from two fused germ cells11.
Fox et al. has proposed the “germ cell theory” as a potential mechanism. He believed that, in the primary phases of embryogenesis, the primitive gut evaginates into the umbilical cord, and germ cells from the gut migrate out and are deposited in the connective tissue of the umbilical cord, leading to the formation of a teratoma of the cord. If the germ cells continue to migrate until they reach the extraplacental membranes, they develop into an extraplacental membrane teratoma between the amnion and chorion12. The germ cell theory is currently more accepted than the “included twin” hypothesis6. Placental teratomas are typically 2 – 11 cm in length4. Microscopy shows mature tissues derived from the three germinative layers, but are lacking well-defined organization13, 14. However, a case was recently reported in which an immature placental teratoma with evidence of necrosis and neuroepithelial elements was mixed with mature and immature tissue of ectodermal and mesodermal origin15. Prenatal diagnosis is possible by ultrasound, and such findings have been described as abnormalities on or adjacent to the placenta. Prenatal diagnosis can be based on various echogenic tissues such as calcifications, fat, and fluid. Calcification differentiates teratoma from other common tumors such as trophoblastic and chorioangioma14. Fetus amorphous is the primary differential diagnosis of placental teratoma and is diagnosed by ultrasound. Typically, no evidence of a skeletal axis is provided in pathology reports6, 14. In 1991, Akimov described a single isolated case of a large placental teratoma that resulted in fetal asphyxia, possibly due to mechanical compression of the umbilical cord16. Consequently, in masses greater than 10 cm, regular prenatal and intrapartum monitoring of fetal wellbeing is recommended due to the potential for fetal hypoxia17. Placental teratoma is a benign tumor that typically has no adverse effect on the mother or fetus, but the potential for malignancy is unknown. Because of its benign features, prenatal diagnosis of other tumors is important. More information is needed on this rare abnormality.
Conclusion
An awareness of placental teratoma is important from a pathological perspective in order to include it as a possibility in the differential diagnosis of benign placental nodules, as well as obtain more information about this unusual aberration, and conduct more studies on this type of prenatal anomaly.
Abbreviations
None.
Acknowledgments
None.
Author’s contributions
All authors equally contributed to the all parts of conceptualization and data collection. All authors read and approved the final draft of the manuscript.
Funding
None.
Availability of data and materials
Data and materials used in the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
This study was conducted in accordance with the amended Declaration of Helsinki. The written informed consent was obtained from the patient.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
-
Ahmed
N.,
Kale
V.,
Thakkar
H.,
Hanchate
V.,
Dhargalkar
P.,
Sonographic diagnosis of placental teratoma. Journal of Clinical Ultrasound.
2004;
32
(2)
:
98-101
.
View Article PubMed Google Scholar -
Meinhard
K.,
Dimitrov
S.,
Nicolov
A.,
Dimitrova
V.,
Vassilev
N.,
Placental teratoma: a case report. Pathology, Research and Practice.
1999;
195
(9)
:
649-51
.
View Article PubMed Google Scholar -
Morville
P.,
Une teratoma placentaire. Gynecol Obstet (Paris).
1925;
2
:
29-32
.
-
Chandy
R.G.,
Korula
A.,
Seshadri
L.,
Teratoma of the placenta. Australian and New Zealand Journal of Obstetrics and Gynaecology.
2002;
42
(5)
:
556-7
.
View Article PubMed Google Scholar -
Elagöz
S.,
Aker
H.,
Cetin
A.,
Placental teratoma. A case report. European Journal of Obstetrics, Gynecology, and Reproductive Biology.
1998;
80
(2)
:
263-5
.
View Article PubMed Google Scholar -
Prashanth
A.,
Lavanya
R.,
Girisha
K.M.,
Mundkur
A.,
Placental Teratoma presenting as a lobulated mass behind the neck of fetus: a case report. Case Reports in Obstetrics and Gynecology.
2012;
2012
:
857230
.
View Article PubMed Google Scholar -
Sarmiento
A.,
Quijano
F.E.,
Puccini
G.,
Rodríguez
N.,
Gómez
P.A.,
Corangioma placentario. Reporte de caso y revisión de la literatura. Revista Colombiana de Obstetricia y Ginecologia.
2008;
59
(1)
:
62-7
.
View Article Google Scholar -
Gruca
K.,
Ropacka
M.,
Breborowicz
G.H.,
Non-trophoblastic placental tumors. Archives of Perinatal Medicine..
2011;
17
:
113-7
.
-
Shimojo
H.,
Itoh
N.,
Shigematsu
H.,
Yamazaki
T.,
Mature teratoma of the placenta. Pathology International.
1996;
46
(5)
:
372-5
.
View Article PubMed Google Scholar -
Geoffrey
H.,
Studies on tumour formation. By G. W. de P. Nicholson, M.A., M.B. , B.Ch., Late Professor of Pathology, Guy's Hospital, London. 1950. London: Butterworth & Co. (Publishers) Ltd. .
.
-
Tavares
A.S.,
On the sex of cancer and teratomata cells. Lancet.
1955;
268
(6871)
:
948-9
.
View Article PubMed Google Scholar -
Fox
H.,
Butler-Manuel
R.,
A teratoma of the placenta. The Journal of Pathology and Bacteriology.
1964;
88
(1)
:
137-40
.
View Article PubMed Google Scholar -
Gaffar
B.A.,
Hotait
H.Y.,
Gamlouch
S.F.,
Swalaha
N.J.,
Placental teratoma or fetus acardius amorphous?. Hematology/Oncology and Stem Cell Therapy.
2008;
1
(1)
:
57-61
.
View Article PubMed Google Scholar -
Kudva
R.,
Monappa
V.,
Rai
L.,
Placental teratoma: a diagnostic dilemma with fetus acardius amorphous. Indian Journal of Pathology & Microbiology.
2010;
53
(2)
:
378-9
.
View Article PubMed Google Scholar -
Shahzadi
S.,
Immature placental teratoma. Journal of Postgraduate Medical Institute.
2014;
28
:
324-7
.
-
Akimov
O.V.,
[Giant teratoma of the placenta (acardius amorphus)]. Arkhiv Patologii.
1991;
53
(4)
:
59-60
.
PubMed Google Scholar -
Tan
G.,
Shiran
M.,
Aireen
I.,
Swaminathan
M.,
Hayati
A.,
Zaleha
A.,
Large teratoma of the Placenta. The Internet Journal of Gynecology and Obstetrics..
2008;
11
:
12
.
Comments
Article Details
Volume & Issue : Vol 9 No 1 (2022)
Page No.: 4818-4821
Published on: 2022-01-22
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 6133 times
- PDF downloaded - 1578 times
- XML downloaded - 0 times
 Biomedpress
Biomedpress



