Abstract
Background: Rheumatoid arthritis (RA) is long-term autoimmune disorder that primarily affects the joints. Vitamin D has a role in the activity and pathogenesis of RA. The aim of this study is to determine the correlation of vitamin D and anti-cyclic citrullinated peptide (anti-CCP) with disease activity in RA patients.
Methods: A case-control study was conducted between November 2021 and February 2022. A questionnaire was designed to obtain demographic and clinical data from both males and females over 18 years old who did not take vitamin D supplements. A total of 142 blood samples were collected in sterile containers from RA patients. Serum vitamin D and anti-CCP levels from cases and control samples were measured using ELISA.
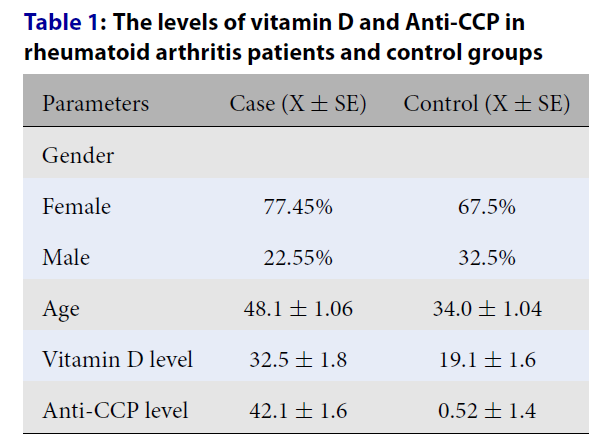
Results: Of the cases, 77.45% were females and 22.55% were males, whereas 67.5% of the controls were females and 32.5% were males. The average age of the cases and controls was 48.1 +/- 1.06 years and 34.0 +/- 1.04 years, respectively. The level of vitamin D was 32.5 +/- 1.8 in the cases and 19.1 +/- 1.6 in the controls. The level of anti-CCP was 42.1 +/- 1.6 in the cases and 0.52 +/- 1.4 in the controls. Vitamin D deficiency level ratio was 21.7% for the cases and 61% for controls, vitamin D insufficiency ratio was 30.4% for the cases and 18% for controls, and vitamin D sufficiency ratio was 47.9% for the cases and 21% for controls.
Conclusions: There was an inverse negative correlation between vitamin D level and disease activity in RA patients.
Introduction
Rheumatoid arthritis (RA) is long-term autoimmune disorder that primarily affects the joints1. Approximately 1% of the population is affected by this disorder, with a ratio of 3:1 in females vs males2. In 2011, nearly 11.9 million people around the world experienced disability caused by RA3. The cause of RA is not clear; however, alcohol consumption4 and silica exposure have been linked to RA5.
Vitamin D is a secosteroid hormone involved in bone and calcium metabolism6. It is produced in the skin under ultraviolet radiation from the pro-vitamin 7-dehydrocholesterol and can be absorbed from food in small amounts7. Limited uptake of calcium and phosphate are correlated with vitamin D deficiency, which leads to a decrease in bone mineralization, bone softening in adults, and rachitis in children shown as clinical symptoms when Vitamin D deficiency occur8, 9.
Vitamin D deficiency has been implicated in the pathogenesis of autoimmune diseases, such as type 1 diabetes and multiple sclerosis. Reduced vitamin D intake has been linked to increased susceptibility to the development of RA, and vitamin D deficiency has been found to be associated with disease activity in patients with RA10. RA is a cardiovascular risk factor. Low serum levels of vitamin D may increase blood pressure and decrease high-density lipoprotein (HDL) cholesterol levels11.
Anti-cyclic citrullinated peptide (anti-CCP) antibodies have been used as highly specific and sensitive markers in the diagnosis of RA in recent years12.
Vitamin D has recently been recognized to have a role in the activity and pathogenesis of RA13. The aim of this study was to determine the correlation of serum vitamin D and anti-CCP antibody levels with disease activity in patients recently diagnosed with RA.
Methods
Study population
A case-control study was conducted to determine the correlation of vitamin D and anti-CCP with disease activity in RA patients. The study population included all RA patients in Khartoum hospitals, both male and female, above 18 years of age who did not take vitamin D supplements.
Inclusion criteria
All RA patients in Khartoum State hospitals (Sudan) above 18 years of age who did not take vitamin D supplements.
Exclusion criteria
Non-RA patients, patients outside of Khartoum State hospitals (Sudan), patients 18 years of age or younger, and patients taking any vitamin D supplements.
Study area and materials
The study was conducted at Al-Rayan Medical Diagnostic Center during the period between November 2021 and February 2022. The material used in the study included multi-channel pipettes and micro-pipettes, an automated wash system, micro-plate reader with 450 nm or 620 – 680 nm filters, and a -20°C refrigerator.
Demographic and clinical data
A questionnaire was designed to obtain demographic and clinical data by direct interview with RA patients in hospitals. The data included age, gender, and whether they took any vitamin D supplements before the study.
Sample collection
A total of 142 blood specimens (n = 142) were collected in sterile containers from RA patients. The serum samples were preserved at -20°C until processing.
Enzyme-linked immunosorbent assay (ELISA)
Vitamin D levels for cases and controls were estimated from the collected serum samples using 25-OH Vitamin D ELISA Diagnostic kits, according to the manufacturer protocol (EUROIMMUN-EQ6411-9601). The concentration of anti-CCP in the samples was measured using ELISA with anti-CCP IgG. The ELISA test kits provided a semi-quantitative or quantitative in vitro assay for the determination of human autoantibodies of the IgG class against CCPs. The assay was performed according to the manufacturer protocol.
Ethics approval and consent to participate
Ethical approval was obtained from the Ministry of Health Ethical Research Committee in accordance with the principles of the Declaration of Helsinki, and permission was granted by hospital administration prior to sample and data collection. The patients’ information was highly secured and not used for purposes other than scientific inquiry.
Each participant was asked to sign a written ethical consent form during the interview, before the specimen was obtained. The informed ethical consent form was designed and approved by the ethical committee of the Ministry of Health, Sudan.
Ethical clearance code number: MH-RES/4-021-07
Date: 8/1/2021
Statistical analysis
Data were analyzed using Statistical Package for Social Sciences (SPSS) software version 20 (IBM Corp., Armonk, NY, USA). Quantitative data are expressed as mean ± standard deviation. Qualitative data are expressed as frequencies and percentages.
| Parameters | Case (X ± SE) | Control (X ± SE) |
|---|---|---|
| Gender | ||
| Female | 77.45% | 67.5% |
| Male | 22.55% | 32.5% |
| Age | 34.0 ± 1.04 | |
| Vitamin D level | 32.5 ± 1.8 | 19.1 ± 1.6 |
| Anti-CCP level | 42.1 ± 1.6 | 0.52 ± 1.4 |
| Items | RA cases group (%) | Control group (%) |
|---|---|---|
| Deficiency ratio | 21.7 | 61 |
| Insufficiency ratio | 30.4 | 18 |
| Sufficiency ratio | 47.9 | 21 |
| Vitamin D deficiency level in males and females | ||
| Gender | Male | Female |
| 27.3 | 28 | |
Results
The characteristics of the cases in the study population were 77.45% female and 22.55% male. Among the control group, 67.5% were female and 32.5% were male. The average age of the cases and controls was 48.1 ± 1.06 years and 34.0 ± 1.04 years, respectively. The level of vitamin D was 32.5 ± 1.8 in the cases and 19.1 ± 1.6 in the control group (p < 0.05). The level of anti-CCP was 42.1 ± 1.6 for the cases and 0.52 ± 1.4 for the controls (p < 0.05) (Table 1).
The prevalence of vitamin D deficiency and insufficiency defined as a 25(OH)-D level < 20 ng/ml and < 30 ng/ml, respectively, are presented in Table 2. The vitamin D deficiency level ratio was 21.7% for cases and 61% for controls (p < 0.05). The vitamin D insufficiency ratio was 30.4% for cases and 18% for controls, whereas the vitamin D sufficiency ratio was 47.9% for cases and 21% for controls. Furthermore, the vitamin D deficiency level was 27.3% in males and 28% in females (p < 0.05) (Table 2).
Discussion
Vitamin D deficiency has been linked to several autoimmune disorders, including insulin-dependent diabetes mellitus, systemic lupus erythematous (SLE), and RA14. Vitamin D has recently been recognized to have a role in the activity and pathogenesis of RA13.
In the present study, vitamin D levels were lower in the healthy population than in the RA patients15. In contrast, vitamin D deficiency in healthy individuals, especially in women, was high, and these individuals did not receive supplementation of 25-OH-D. The main reasons for the high prevalence of 25-OH deficiency in the healthy population is that Sudan is geographically located in North Africa, and the natural pigmentation (melanin) in skin color (black) is associated with reduced vitamin D production in the skin of this population. In addition, the median vitamin D intake of people in our country is below the recommended intake in every age group, with or without the inclusion of vitamin D from supplements. Second, lifestyle may account for this deficiency: reduced outdoor activities and environmental factors (e.g., air pollution) that reduce exposure to sunlight, which is required for ultraviolet B (UVB)-induce vitamin D production in the skin. Third, there is a lack of access to 25-OH-D-enriched food products, such as cod liver oil, swordfish, salmon, canned tuna, beef liver, egg yolks, and mushrooms in our country. Lack of access to 25-OH-D-enriched food sources leads to nutritional 25-OH-D deficiency.
In this study, 21.7% of RA patients had vitamin D deficiency. In a recent study, vitamin D deficiency prevalence was reported to be 48.7%9. We demonstrated a weak positive correlation between age and anti-CCP levels among RA patients. There was a significant difference between genders among the case and control groups: females were more affected by RA disease than men2. Similarly, the incidence of vitamin D deficiency was higher in females than males. Vitamin D concentrations were lower in patients with newly diagnosed RA when compared with other patients.
Correlation co-efficient analysis of serum 25-OH-D was -0.323 using multiple linear regression, indicating that there was an inverse relationship between serum 25-OH-D levels and the severity of RA (p=0.001). These finding are in line with studies conducted by Wang et al.16 and Maurizio Rossini17.
Kostoglou-Athanassiou et al. reported that vitamin D deficiency was highly prevalent in patients with RA and that vitamin D deficiency may be linked to disease severity in RA. As vitamin D deficiency has been associated with diffuse musculoskeletal pain, these results have therapeutic implications. Vitamin D supplementation may be needed both for the prevention of osteoporosis and for pain relief in patients with RA10.
Lee and Bae reported that serum vitamin D levels were low in patients with RA, vitamin D deficiency was prevalent in RA patients, and vitamin D level correlated inversely with RA activity. The results of our meta-analysis suggest that vitamin D level is associated with susceptibility to RA and RA activity18. Cecchetti et al., reported that vitamin D was inversely correlated with RA activity and body mass index11.
A previous study revealed that anti-CCP and rheumatoid factor titers may be valuable in the estimation of disease activity and other inflammatory parameters in RA patients19. Antibodies against CCP were thought to be more specific than rheumatoid factor in RA, and the determination of anti-CCP in addition to rheumatoid factor could be helpful in serological diagnosis and monitoring of patients with RA12. Hayashi et al., reported that anti-CCP was superior to other biomarkers in terms of diagnostic accuracy and that these combined assays were useful in the early diagnosis of RA20.
A small sample size and the samples being taken only from Khartoum State in Sudan, not including other cities, were the limitations of this study.
Conclusions
There was a negative inverse correlation between vitamin D level and disease activity in RA patients.
Abbreviations
Anti-CCP: Anti-cyclic citrullinated peptide, ELISA: Enzyme-linked immunosorbent assay, RA: Rheumatoid arthritis, SLE: systemic lupus erythematous UVB: Ultraviolet-B
Acknowledgments
Thanks for all participants involved in this research.
Author’s contributions
EFM and ASI conceived the design and carried out the experiments. MYA obtained, analyzed and interpreted the data. LAM and HHM wrote and revised the manuscript. AAI provides financial support for all experiments. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
All authors read and approved the final manuscript.
Funding
Not applicable.
Availability of data and materials
Data and materials used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
Each participant was asked to sign a written ethical consent form during the interview, before the specimen was taken. The informed ethical consent form was designed and approved by the ethical committee of the Ministry of Health -Sudan.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
-
“Hand out on Health: Rheumatoid arthritis”. National Institute of Arthritis and Musculoskeletal and skin disease. August 2014. https://www.niams.nih.gov/.
.
-
World Health Organization. Principle and method for assessing auto-immunity associated with exposure to chemicals. 2006. https://apps.who.int/iris/handle/10665/43603?locale-attribute=de&. 2006
.
-
Krahn
G.L.,
WHO World report on disability: a review. Disability and Health Journal.
2011;
4
(3)
:
141-2
.
View Article PubMed Google Scholar -
Liao
K.P.,
Alfredsson
L.,
Karlson
E.W.,
Environmental influences on risk for rheumatoid arthritis. Current Opinion in Rheumatology.
2009;
21
(3)
:
279-83
.
View Article PubMed Google Scholar -
Pollard
K.M.,
Silica, Silicosis, and Autoimmunity. Frontiers in Immunology.
2016;
7
:
97
.
View Article PubMed Google Scholar -
Holick
M.F.,
Vitamin D: evolutionary, physiological and health perspectives. Current Drug Targets.
2011;
12
(1)
:
4-18
.
View Article PubMed Google Scholar -
Holick
M.F.,
Binkley
N.C.,
Bischoff-Ferrari
H.A.,
Gordon
C.M.,
Hanley
D.A.,
Heaney
R.P.,
Endocrine Society
Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. The Journal of Clinical Endocrinology and Metabolism.
2011;
96
(7)
:
1911-30
.
View Article PubMed Google Scholar -
Pludowski
P.,
Holick
M.F.,
Grent
W.B.,
Konstanynowicz
J.,
Povoroznyuk
V.,
Balatska
N.,
Vitamin D supplementation guidelines. J Steroid Biochem Mol Biol.
2018;
175
:
125-35
.
View Article PubMed Google Scholar -
EFSA panel on Dietetic products. Nutrition and Allergies (NDA). Dietary reference Values for vitamin D. EFSA Journal.
2016;
14
(10)
:
145
.
-
Kostoglou-Athanassiou
I.,
Athanassiou
P.,
Lyraki
A.,
Raftakis
I.,
Antoniadis
C.,
Vitamin D and rheumatoid arthritis. Therapeutic Advances in Endocrinology and Metabolism.
2012;
3
(6)
:
181-7
.
View Article PubMed Google Scholar -
Cecchetti
S.,
Tatar
Z.,
Galan
P.,
Pereira
B.,
Lambert
C.,
Mouterde
G.,
Prevalence of vitamin D deficiency in rheumatoid arthritis and association with disease activity and cardiovascular risk factors: data from the COMEDRA study. Clinical and Experimental Rheumatology.
2016;
34
(6)
:
984-90
.
PubMed Google Scholar -
Aridoğan
B.C.,
Kaya
S.,
Savaş
S.,
Cetin
E.S.,
Akkuş
S.,
Demirci
M.,
Romatoid artritin serolojik tanisinda ve hastalik aktivitesinin değerlendirilmesinde anti-CCP (cyclic citrullinated peptide) antikorlarinin rolü. Mikrobiyoloji Bulteni.
2008;
42
(4)
:
669-74
.
PubMed Google Scholar -
Song
G.G.,
Bae
S.C.,
Lee
Y.H.,
Association between vitamin D intake and the risk of rheumatoid arthritis: a meta-analysis. Clinical Rheumatology.
2012;
31
(12)
:
1733-9
.
View Article PubMed Google Scholar -
Jankosky
C.,
Deussing
E.,
Gibson
R.L.,
Haverkos
H.W.,
Viruses and vitamin D in the etiology of type 1 diabetes mellitus and multiple sclerosis. Virus Research.
2012;
163
(2)
:
424-30
.
View Article PubMed Google Scholar -
Sahebari
M.,
Mirfeizi
Z.,
Rezaieyazdi
Z.,
Rafatpanah
H.,
Goshyeshi
L.,
25(OH) vitamin D serum values and rheumatoid arthritis disease activity (DA S28 ESR). Caspian Journal of Internal Medicine.
2014;
5
(3)
:
148-55
.
PubMed Google Scholar -
Wang
Y.,
Zhang
F.,
Wang
S.,
Shang
X.,
Luo
S.,
Zhou
H.,
Serum Vitamin D Level is Inversely Associated With Anti-Cyclic Citrullinated Peptide Antibody Level and Disease Activity in Rheumatoid Arthritis Patients. Archives of Rheumatology.
2015;
31
(1)
:
64-70
.
View Article PubMed Google Scholar -
Rossini
M.,
Maddali Bongi
S.,
La Montagna
G.,
Minisola
G.,
Malavolta
N.,
Bernini
L.,
Vitamin D deficiency in rheumatoid arthritis: prevalence, determinants and associations with disease activity and disability. Arthritis Research {&}amp; Therapy.
2010;
12
(6)
:
216
.
View Article PubMed Google Scholar -
Lee
Y.H.,
Bae
S.C.,
Vitamin D level in rheumatoid arthritis and its correlation with the disease activity: a meta-analysis. Clinical and Experimental Rheumatology.
2016;
34
(5)
:
827-33
.
PubMed Google Scholar -
Shakiba
Y.,
Koopah
S.,
Jamshidi
A.R.,
Amirzargar
A.A.,
Massoud
A.,
Kiani
A.,
Anti-cyclic citrullinated peptide antibody and rheumatoid factor isotypes in Iranian patients with rheumatoid arthritis: evaluation of clinical value and association with disease activity. Iranian Journal of Allergy, Asthma, and Immunology.
2014;
13
(3)
:
147-56
.
PubMed Google Scholar -
Hayashi
N.,
Nishimura
K.,
Kumagai
S.,
[New biomarkers for rheumatoid arthritis]. Rinsho Byori.
2008;
56
(4)
:
297-308
.
PubMed Google Scholar
Comments
Article Details
Volume & Issue : Vol 9 No 7 (2022)
Page No.: 5149-5153
Published on: 2022-07-31
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 5077 times
- PDF downloaded - 1499 times
- XML downloaded - 0 times
 Biomedpress
Biomedpress

