Abstract
Obturator hernia is a rare cause of acute abdomen resulting from a protrusion of intra-abdominal contents through the obturator foramen in the pelvis. Obturator hernia is often seen in older adults, emaciated individuals, and chronically ill women. The preoperative diagnosis of obturator hernia is frequently delayed because its nonspecific signs and symptoms complicate the diagnostic process, leading to high mortality rates. The most common clinical presentation of obturator hernia is intestinal obstruction with nausea, vomiting, and abdominal pain. Symptoms caused by the compression and irritation of the obturator nerve within the canal are less common. Open or laparoscopic surgery is the only available treatment; it allows abdominal cavity exploration and hernia reduction. The widespread and increasing use of computed tomography has played an important role in diagnosing conditions. Here, we present the case of a 90-year-old woman diagnosed with strangulated obturator hernia and coronavirus disease 2019 (COVID-19) who underwent emergency surgery at Hanoi Medical University Hospital. We emphasize the role of computed tomography in establishing a prompt preoperative diagnosis and planning an appropriate surgical intervention for this rare condition.
Introduction
Obturator hernia represents <1% of all hernias, indicating its rarity. Because this presentation is challenging to diagnose and treat early, approximately half (47%) of obturator hernia patients are first diagnosed when complications arise or death occurs1. Also known as the "little old lady's hernia," obturator hernia is more common in older women with a low body mass index (BMI) and concurrent medical conditions. The reason for this sex bias is that women have a wider pelvis and a more triangular obturator canal with a greater transverse diameter. Patients with obturator hernia present with acute cases of intestinal obstruction, which can include abdominal pain and distention, nausea, vomiting, and abdominal discomfort. According to the literature, there are three signs specific to a strangulated obturator hernia compressing the obturator nerve. The first, obturator neuralgia, can present as either hyper- or hypoesthesia extending from the inguinal crease to the anteromedial aspect of the thigh. Related to obturator neuralgia, the Howship–Romberg sign, characterized by pain along the distribution of the anterior division of the obturator nerve, is the second specific symptom. Another finding that can be present is the Hannington–Kiff sign, characterized by the absence of the adductor thigh reflex2. Abdominal computed tomography (CT) is an imaging method with high sensitivity and specificity in preoperative diagnosis that allows assessment of the perfusion status of the hernia viscera and other abdominal organs, helping the surgeon develop the most appropriate treatment strategy3. The only treatment method for obturator hernia is surgical, either open or laparoscopic, with abdominal or preperitoneal access to the hernia hole. The hernia defect is repaired by simple sutures, shaped by muscle flaps, or reinforced with artificial materials4.
Here, we present the case of a patient with coronavirus disease 2019 (COVID-19) who was admitted to the hospital with acute intestinal obstruction symptoms and diagnosed with strangulated obturator hernia by abdominal CT scan. The patient underwent successful emergency laparoscopic surgery at the Department of General Surgery, Hanoi Medical University Hospital.
CASE REPORT
The patient was a 90-year-old woman with a history of open appendectomy (McBurney’s incision), hypertension, and heart failure. She presented to the emergency ward with abdominal pain and vomiting that had persisted for 1 day. On arrival, the patient’s general condition was weak, and she demonstrated hypertension (170/90 mmHg) and tachycardia (100 bpm). Her weight was 30 kg, and her height was 145 cm (BMI = 14.3 kg/m2). The local examination revealed central distension of the abdomen with generalized tenderness and guarding. Her other systems appeared normal, and the per rectal and per vaginal examination findings were unremarkable.
The patient tested positive for COVID-19 with a rapid test. Investigations revealed a normal white blood cell (WBC) count of 7.67 G/L, an increased neutrophil count (NEUT) of 87.3%, and C-reactive protein (CRP) levels of 4.37 mg /dL. A bedside abdominal ultrasound revealed dilatation with fluid stagnation in the intestinal loops around the umbilicus; the thickest area of abdominal free fluid measured 15 mm. Moreover, a CT scan revealed left-sided obturator foramen hernia containing a segment of distal ileum causing high-grade small bowel obstruction, reaching 4 cm, and the intestinal loop wall was poorly perfused (Figure 1). Numerous signs of strangulation and ischemia of the bowel were present, including mesenteric edema and bowel wall thickening with decreased enhancement. Echocardiography revealed left ventricular systolic function (ejection fraction) of 43%, and a chest X-ray showed a large heart shadow.
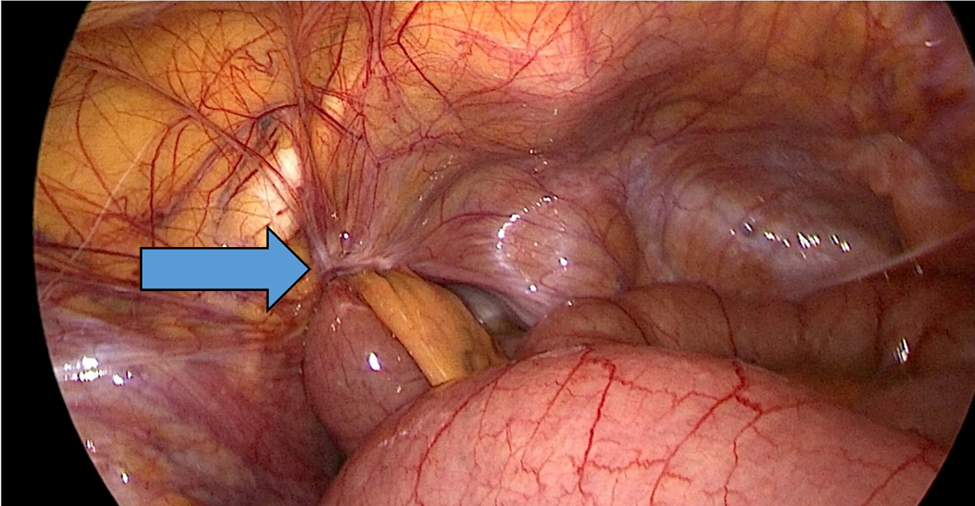
Following a diagnosis of left-sided strangulated obturator hernia with heart failure and COVID-19, the patient was transferred as an emergency case to the operating room 7 hours after admission and 24 hours after symptom onset. A laparoscopic procedure was performed with three small incisions: 5 mm and double 10 mm port-sizes located supraumbilically at the right iliac fossa and the left midclavicular line, respectively. A diagnostic laparoscopy was performed after peritoneal penetration and gas insufflation, and the obturator hernia with bowel content was visualized (Figure 2). A transitional zone at the hernia site showed proximal dilatation and distal collapse of the small bowel.
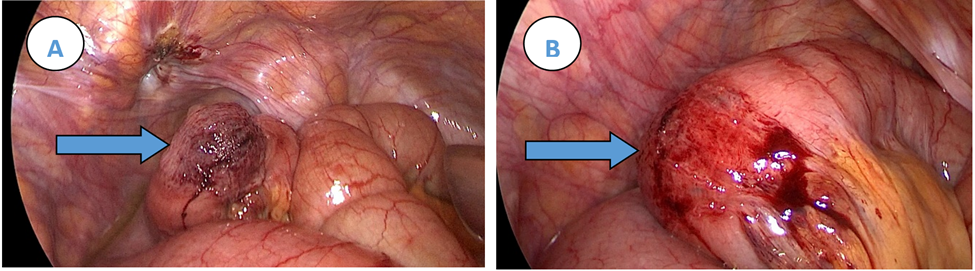
The hernia was subsequently reduced, with signs of bowel ischemia. After 5 minutes, the affected ileal segment appeared healthy (Figure 3). Finally, the entire small bowel was assessed to eliminate any other transitional zones or pathology, and the findings were unremarkable.
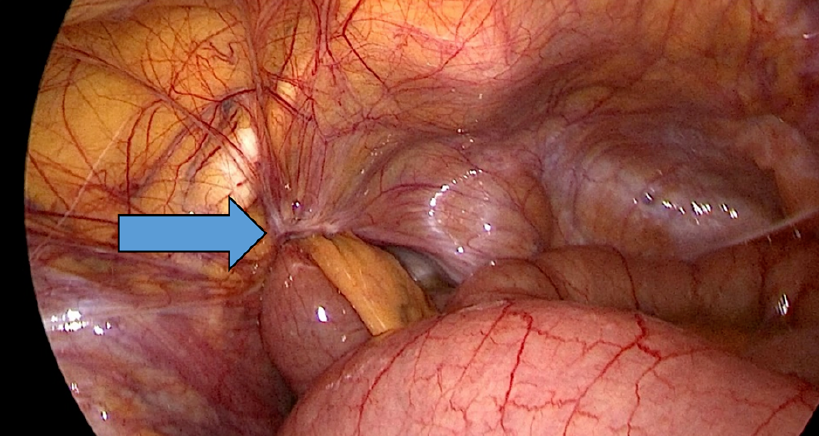
Therefore, as there was no contamination, ischemia, or perforation, suture repair was performed with non-absorbable multifilament Ti-cron™ 2.0 using a double-layer technique. The first layer resulted in the closure of the defect, and the second created a peritoneal plug to fill the defect and reduce the recurrence risk (Figure 4). The surgery time was 45 minutes, and the total anesthesia time was 60 minutes. After 12 hours, the patient could eat, and she was transferred to the medical ward for cardiovascular disease and COVID-19 treatment the following day.
DISCUSSION
Arnaud de Ronsil first described obturator hernia in 1724, and the first successful surgery was performed by Henry Obre in 1851. The condition has remained a rare pathology, accounting for 0.07–1% of all hernias, only 0.2–1.6% of which cause mechanical bowel obstruction4, 5. Obturator hernia commonly affects individuals aged 75 to 90 years, and the incidence in women is nine times higher than that in men1, 6.
The obturator is located between the anterior flexor and posterior extensor muscles in the inner third of the upper thigh. The obturator is an opening of the pelvis. Its upper and lower borders are two branches of the pubic bone, the hip joint and the top of the femur are outside the obturator, and the pubic joint is inside. The sealing membrane covers the sealing hole, except for at the upper and outer positions, where the origin of the obturator tube remains uncovered. The obturator tube is 2–3 cm in length and 1 cm wide, starting from the opening of the sealing membrane, continuing downward, and ending at the obturator area. The components passing through the obturator duct include the obturator nerve bundle and the corpus adiposum, a fatty tissue that fills the obturator duct to prevent any other organs from entering the duct. Patients with obturator hernia are usually older women with low BMI and low body fat percentage, leading to hypoplasia of fat corpuscles and hollowing of the obturator tube, allowing the herniation of internal organs.
Our patient was a 90-year-old woman with a BMI of 14.3 kg/m2, a long history of heart failure, and concurrent COVID-19 infection (during the fourth wave of COVID-19 in Vietnam) accompanied by nonspecific clinical signs. CT is the gold standard for diagnosing obturator hernia preoperatively, especially in early diagnosis, to ensure prompt treatment decision-making to prevent complications and death due to delayed intervention7. Because our patient tested positive for COVID-19, performing a CT scan required adherence to the principles of epidemic prevention despite the knowledge that a delay in intervention could aggravate the patient’s bowel congestion. We ordered an early CT scan as soon as possible after the ultrasound revealed signs of abdominal obstruction that could not be explained, mobilizing a team and securing a separate imaging room to prevent COVID-19 spread.
The patient underwent surgery 7 hours after admission. Considering the patient's cardiovascular status, we chose laparoscopic surgery with abdominal pressure of 10 mmHg. The patient had a health status classification (ASA) score of III. Heart failure and COVID-19 were challenges for both anesthesia and laparoscopic surgery. Open surgery is most often reported in the literature for obturator hernia repair; however, we performed the laparoscopic approach to diagnose, reduce, and repair the obturator hernia in our patient. This minimally invasive approach benefits high-risk patients through reduced postoperative pain, less ileus, fewer pulmonary complications, and a shorter hospital stay. Regardless of the approach, the emphasis should be on rapid evaluation, adequate resuscitation, and early operative intervention to reduce morbidity and mortality rates.
Intraoperatively, the lesion was a Richter-type herniation of a loop of small bowel into the left obturator. The herniated bowel showed signs of ischemia but not necrosis and was preserved after 5 minutes8. In a 2021 study evaluating 10 years of emergency surgical treatment for obturator hernias at 10 major Australian surgical centers, a total of 18 patients had small bowel hernia content, of which nearly 90% had intestinal ischemia, and nearly one-third required intestinal resection (27.8%), with a mortality rate of 27.8%9. In our patient, although surgery was performed almost 24 hours after symptom onset, the bowel segment was preserved. This result may have been due to the small inner hole diameter of the obturator, partially herniated bowel loop, free margin, good blood supply to the mesentery, and timely diagnosis and surgery. This good result further confirms that early diagnosis and intervention are critical factors affecting the prognosis of obturator hernia patients and preventing the need for intestinal resection and other unfortunate complications that often occur in high-risk patients5.
Hernia closure options include simple suturing, placing an artificial mesh, or using a roll of mesh to seal the hernia4, 9. Suture alone has the advantage of being fast and eliminates the potential risk of contamination associated with artificial materials. However, because the anatomical structure of the obturator tube includes mainly hard bone and the obturator membrane, it is sometimes challenging to affix the obturator membrane to the periosteum. We chose this method for two reasons: first, the risk of infection is high if artificial materials are used to treat a hernia loop that has persisted for over 6 hours, and second, the patient’s overall poor body condition necessitated minimizing the surgery time. The surgery lasted 45 minutes, which is much shorter than the previously reported average surgery time10. After surgery, the patient recovered from anesthesia, started eating the next day, and began medical treatment for her cardiovascular disease and COVID-19. The patient reported no complications after surgery and was promptly treated for COVID-19 and cardiovascular disease. She was discharged from the hospital after 10 days of treatment.
CONCLUSION
Obturator hernia is a challenging diagnosis with high morbidity and mortality rates. Obturator hernia should be considered in older female patients with low BMI admitted to the hospital with signs of mechanical high bowel obstruction. CT is a valuable preoperative diagnostic tool for obtaining a definitive diagnosis and determining an early surgical intervention plan. Laparoscopic surgery has many advantages for patients and produces good postoperative results, facilitating the subsequent prompt and successful treatment of COVID-19 and other underlying diseases.
Abbreviations
ASA: American Society of Anesthesiologists, BMI: body mass index, COVID-19: Coronavirus Disease 2019, CRP: C-reactive protein, CT: computed tomography, WBC: white blood cell
Acknowledgments
None.
Author’s contributions
Tran ND, Nguyen DA, and Nguyen MD: Case file retrieval and case summary preparation. Tran ND, Nguyen DA, and Nguyen MD: preparation of manuscript and editing. All authors read and approved the final manuscript.
Funding
None.
Availability of data and materials
Data and materials used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
Our institution does not require ethical approval for reporting individual cases or case series. Written informed consent was obtained from the patient(s) for their anonymized information to be published in this article.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
References
-
Susmallian
S.,
Ponomarenko
O.,
Barnea
R.,
Paran
H.,
Obturator hernia as a frequent finding during laparoscopic pelvic exploration: A retrospective observational study. Medicine.
2016;
95
(27)
:
e4102
.
View Article PubMed Google Scholar -
Petrie
A.,
Tubbs
R.S.,
Matusz
P.,
Shaffer
K.,
Loukas
M.,
Obturator hernia: anatomy, embryology, diagnosis, and treatment. Clinical Anatomy (New York, N.Y.).
2011;
24
(5)
:
562-9
.
View Article PubMed Google Scholar -
Nishina
M.,
Fujii
C.,
Ogino
R.,
Kobayashi
R.,
Kumada
K.,
Yamane
K.,
Preoperative diagnosis of obturator hernia by computed tomography. Seminars in Ultrasound, CT, and MR.
2002;
23
(2)
:
193-6
.
View Article PubMed Google Scholar -
Park
J.,
Obturator hernia: clinical analysis of 11 patients and review of the literature. Medicine.
2020;
99
(34)
:
e21701
.
View Article PubMed Google Scholar -
Kulkarni
S.R.,
Punamiya
A.R.,
Naniwadekar
R.G.,
Janugade
H.B.,
Chotai
T.D.,
Vimal Singh
T.,
Obturator hernia: A diagnostic challenge. International Journal of Surgery Case Reports.
2013;
4
(7)
:
606-8
.
View Article PubMed Google Scholar -
Gilbert
J.D.,
Byard
R.W.,
Obturator hernia and the elderly. Forensic Science, Medicine, and Pathology.
2019;
15
(3)
:
491-3
.
View Article PubMed Google Scholar -
Khaladkar
S.M.,
Kamal
A.,
Garg
S.,
Kamal
V.,
Bilateral obturator hernia diagnosed by computed tomography: a case report with review of the literature. Radiology Research and Practice.
2014;
2014
:
625873
.
View Article PubMed Google Scholar -
Hayes
C.,
Schmidt
K.,
Neduchelyn
Y.,
Ivanovski
I.,
Obturator hernia of Richter type: a diagnostic dilemma. BMJ Case Reports.
2020;
13
(12)
:
e238252
.
View Article PubMed Google Scholar -
Diab
J.,
Badiani
S.,
Berney
C.R.,
A decade review of emergency obturator hernia repairs. ANZ Journal of Surgery.
2021;
91
(7-8)
:
1596-603
.
View Article PubMed Google Scholar -
Liu
J.,
Zhu
Y.,
Shen
Y.,
Liu
S.,
Wang
M.,
Zhao
X.,
Nie
Y.,
Chen
J.,
The feasibility of laparoscopic management of incarcerated obturator hernia. Surgical endoscopy.
2017;
31
:
656-660
.
View Article Google Scholar
Comments
Article Details
Volume & Issue : Vol 10 No 4 (2023)
Page No.: 5619-5623
Published on: 2023-04-30
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 4967 times
- PDF downloaded - 1514 times
- XML downloaded - 127 times
 Biomedpress
Biomedpress