Abstract
Platelet-rich plasma (PRP) therapy has gained popularity as a treatment option for osteoarthritis, despite a lack of formal endorsement by professional associations. While not universally recommended, its application in managing joint osteoarthritis and aiding ligament regeneration has received approval in several countries. Research into PRP's effectiveness in treating joint osteoarthritis presents promising outcomes, but suffers from inconsistencies across various studies. These disparities stem from differences in the methods of PRP preparation, the concentration of platelets, the frequency of injections, and the specific type of PRP utilized. This article aims to provide the most recent insights into the efficacy of PRP therapy for joint osteoarthritis, underscoring the significant impact of PRP classification, platelet dosage, and injection regimen on therapeutic outcomes. In sum, findings from this study advocate for the use of PRP in managing joint osteoarthritis, highlighting its potential benefits when applied under optimized conditions.
Introduction
Platelet-rich plasma (PRP) is a common concept in medicine. The concept and description of PRP has been around since 1970, when hematologists created products with higher platelet levels than normal blood levels to treat platelet deficiency diseases1. Ten years later, platelet-rich fibrin (PRP) was used for facial surgery1. PRP is an anti-inflammatory agent that stimulates cell proliferation.
Subsequently, PRP was mainly used in the field of musculoskeletal medicine to treat sports injuries. Since its use by professional athletes, PRP has become widely known in the media and widely used in this field. Other medical fields, such as cardiovascular surgery, pediatric surgery, internal surgery, soft tissue surgery, cosmetic anatomy, and ophthalmology, have also used PRP. Recently, many publications have shown that PRP is widely used in the field of cosmetic dermatology, especially in tissue regeneration, treating acne scars, and skin rejuvenation2, 3, 4, 5, 6. Some studies have shown that PRP is also used to treat reproductive disorders, especially early ovarian failure or thickening of the endometrium, in patients who have failed to implant multiple times7, 8.
The use of PRP in treating osteoarthritis is a prominent application of autologous PRP, and many studies have shown the effects of PRP on pain reduction, inflammation reduction, and cartilage regeneration has been reported9, 10, 11. Many studies have compared the therapeutic effects of PRP with corticoid column injection or HA hyaluronic acid solution, showing the advantages of platelet-rich plasma therapy compared to other methods.
Platelets are one of the three types of blood cells produced from the bone marrow and play important roles in the coagulation process and tissue regeneration. The role of platelets in healing depends on the growth factors contained within platelets. When activated, they release these factors to participate in coagulation and wound healing. Platelet factors belong to two main groups: growth factors and cytokines. These factors affect inflammatory processes, angiogenesis, cell migration, and cell proliferation12, 13, 14, 15, 16. Therefore, platelet-rich plasma is a source of natural growth factors that are used for tissue regeneration. Some important growth factors of platelets include: vascular endothelial growth factor (VEGF), platelet-derived growth factor (PDGF), fibroblast growth factor (FGF), epidermal growth factor (EGF), hepatocyte growth factor (HGF), insulin-like growth factors 1 and 2 (IGF-1, 2)...17
This article aims to systematically synthesize the most recent research results from scientists and research groups worldwide on the use of PRP in the treatment of inflammatory arthritis and degenerative arthritis. This article provides clear evidence with updated clinical research results to support the use of PRP in treating degenerative arthritis under the condition that professional associations have not yet determined PRP as a mainstream treatment method for degenerative arthritis.
New evidence from meta-analyses
Belk et al. (2023) conducted a meta-analysis based on 17 studies (Group I, Level I) involving 1042 patients with osteoarthritis treated with PRP injections, 226 patients treated with Bone Marrow Aspirate Concentrate (BMAC) injections, and 1128 patients treated with Hyaluronic Acid (HA) injections. The meta-analysis results showed that PRP injections were more effective post-injection than HA injections, especially in terms of WOMAC and VAS indices. The results also indicated no significant difference between the effectiveness of PRP and BMAC18. The analysis by Veronesi et al. (2023) demonstrated that injections of PRP and the stromal vascular fraction (SVF) were equally effective19.
Qiao et al. (2023) analyzed and compared the treatment effectiveness of osteoarthritis of the knee using PRP injections versus corticosteroid, HA, and a combination of HA and PRP injections20. The analysis of 35 studies with 3104 participants showed that the best treatment effectiveness was in the group receiving PRP or PRP combined with HA. Use of HA or corticosteroids alone was less effective, with much lower improvements in VAS and WOMAC scores compared to PRP or PRP + HA after 12 months. Specifically, the best VAS scores were observed in the PRP group, followed by the PRP+HA, HA, and corticosteroid groups20. These observations were confirmed in a recent study by Khalid et al. (2024)21. Khalid et al. (2024) performed a meta-analysis of 42 studies involving 3696 patients with knee osteoarthritis treated with PRP, HA, and corticosteroids. Based on the VAS and WOMAC score analysis, Khalid et al. (2024) also confirmed that PRP injections were better than HA and corticosteroid injections for up to 12 months21. In newly published meta-analyses, Wang et al. (2024) and Oeding et al. (2024) also confirmed that PRP injections were better than corticosteroid injections22, 23.
Notably, in a recent publication by Gesheff et al. (2024), the authors compared the time from intra-articular injections of PRP, HA, or corticosteroids to the need for total knee replacement24. The authors found that 2.2% of patients treated with PRP would require total knee replacement (71 of 3240 patients), 5.9% of patients treated with corticosteroids would require total knee replacement (13,044 of 1,382,572 patients), and 8.0% of patients treated with HA would require total knee replacement (13,044 of 164,000 patients)24. However, because of the smaller number of patients treated with PRP than those treated with HA and corticosteroids, the authors did not compare the time from intra-articular injections to the need for total knee replacement. The time from the first HA injection to the need for total knee replacement and the time from the first corticosteroid injection to the need for total knee replacement were almost the same (377.8 days in the HA group versus 370.0 days in the corticosteroid group, p = 0.05).
Factors Affecting the Efficacy of PRP Treatment
Platelet Count
In a recent publication, Hohmann (2024) suggested that a high platelet dose would be an effective treatment for osteoarthritis25. Hohmann proposed that a dose of fewer than 2.5 billion platelets is ineffective25, while a dose of more than 5 billion platelets yields good results both 6 and 12 months post-treatment. However, the publication also mentioned that questions remain about whether PRP needs activation, the optimal dose, injection frequency, platelet separation methods, etc., which are still unclear25. Hohmann's suggestion is consistent with the results of an earlier study conducted by Patel et al. (2024). In a triple-blind clinical study, Patel et al. (2024) compared the treatment efficacy of a 2.82 billion platelets dose against a 5.65 billion platelets dose for knee osteoarthritis. Although patients from both groups showed improvement in scores compared to before treatment, a better outcome was recorded in the group receiving a higher platelet dose (p < 0.001). Patient satisfaction with treatment results after 6 months also showed a significant difference, with 96% of patients treated with the higher dose satisfied compared to 68% of patients treated with the lower platelet dose26.
These results were confirmed by a recent study27. Berrigan et al. (2024) analyzed 29 studies and showed that the studies concluding beneficial effects of PRP injections used an average platelet dose of over 5 billion platelets (5.464 ± 511), whereas the studies reporting no statistical difference used a platelet dose of only 2 billion platelets (2.253 ± 753)27. Indeed, the study by Bennell et al. (2021) was among those who did not support the use of PRP in the treatment of knee osteoarthritis28. In this study, the research group was injected with LP-PRP three times consecutively over three weeks compared to the control group (saline injection). The results showed no differences in symptoms or joint structures after 12 months28. The reason for this non-responsiveness to treatment in this study might be the platelet dose. According to the data provided by the authors, the platelet dose used was relatively low, averaging 1.6 billion platelets in 5 mL PRP28.
In particular, in the study by Bansal et al. (2021) conducted on patients with Grade III knee osteoarthritis (over 80% of patients with Grade III knee osteoarthritis), the research group used a very high platelet dose (10 billion platelets in 8 mL injection)29. The results showed that in patients with Grade III knee osteoarthritis, PRP injections were also effective, with a significant reduction in WOMAC score, an increase in IKDC score, and an increase in 6-min pain-free walking distance after 1 year. This study also affirmed that the effectiveness of treatment does not depend on the number of platelet enrichment processes or platelet density but solely on the total number of platelets29.
Type of PRP
The treatment efficacy of PRP depends not only on the number of platelets within the preparation but also on the type of PRP. Currently, based on the presence of leukocytes within PRP preparations, scientists classify PRP into three main types: Pure PRP, Leukocyte-Poor PRP (LP-PRP), and Leukocyte-Rich PRP (LR-PRP). According to Xiong et al. (2023), a meta-analysis of 24 Randomized Controlled Trials (RCTs) showed that the treatment efficacy of LP-PRP was better than that of LR-PRP in the treatment of osteoarthritis30. However, another analysis by Kim et al. (2023) showed that both LP-PRP and LR-PRP resulted in improved joint pain compared to Hyaluronic Acid (HA) injections31. However, in this analysis, Kim et al. reported no difference in pain and swelling between LP-PRP and HA injections, but LR-PRP injections caused pain and swelling related to the injection procedure (with an odds ratio of 3.3). This observation was analyzed by Kim et al. (2023) in 21 level 1 RCTs involving 1077 PRP joint injections and 1009 HA joint injections. A previous publication by Kim et al. (2021) also stated that LR-PRP injections cause more pain and swelling than LP-PRP injections32. Chen et al. (2023) also found LP-PRP to be better than LR-PRP in changing the IKDC scores in treating knee osteoarthritis33. However, another pooled analysis by Abbas et al. (2023) suggested no significant difference in the treatment of knee osteoarthritis between LP-PRP and LR-PRP34.
Activated PRP
The activation of PRP before injection also affects treatment efficacy for knee osteoarthritis. To clarify this, Simental-Mendia et al. (2022) performed a meta-analysis of clinical studies divided into two groups: those using activated PRP and those using non-activated PRP. The authors summarized 14 RCTs with a total of 1292 patients in both groups: the group using activated PRP and the group using non-activated PRP. The results showed that exogenous (pre-activation) activated PRP is more effective in improving pain and functional scores in treating knee osteoarthritis35.
Repeat Injections
Tao et al. (2023) analyzed 7 studies with 575 patients to compare the efficacy of injecting 1 dose, 2 doses, and 3 doses of PRP. The results showed that injecting three doses of PRP significantly improved the VAS score after 12 months (p < 0.0001), whereas injecting two doses and one dose resulted in similar outcomes after 12 months of injection36. Recently, Zhuang et al. (2024) compared the response to 1, 3, and 5 doses of PRP in the treatment of knee osteoarthritis in 106 patients. The research group showed that injecting three or five doses of PRP is safe and more effective than a single injection in improving joint pain, joint function, and motor function in patients with Grade I-III knee osteoarthritis. However, the study showed no significant difference between three and five injections. Therefore, the research group suggested that three injections are necessary to achieve optimal efficacy in treating knee osteoarthritis37.
In 2023, Saraf et al. conducted a randomized controlled clinical trial to evaluate the effectiveness of three consecutive PRP injections (one injection each month) in treating Grade II and III knee osteoarthritis (Kellgren-Lawrence scale)38, 39. In this study, 31 patients received three PRP injections and 27 received saline injections. The results confirmed that at 3, 6, and 12 months, 3 consecutive PRP injections significantly improved VAS, WOMAC in patients with Grade II and III knee osteoarthritis compared to the saline injection group (p < 0.05)38. Li et al. (2023) compared the efficacy of multiple PRP injections versus multiple HA injections in the knee was evaluated by Li et al. (2023) in a recent pooled analysis. Li et al. (2023) analyzed 14 RCTs with 1512 patients. The efficacy of multiple PRP injections was compared with that of multiple HA injections based on VAS, WOMAC, IKDC, or EQ-VAS scores. At 1, 3, 6, and 12 months, multiple PRP injections significantly changed VAS, WOMAC, IKDC, and EQ-VAS scores39. At 3 and 12 months, the VAS score in the group with multiple PRP injections was significantly lower than that in the group with multiple HA injections (P < 0.00001). Furthermore, the WOMAC score in the group with multiple PRP injections was significantly lower than that in the HA multiple injection group at 1, 3, 6, and 12 months (p < 0.01). Meanwhile, the IKDC score significantly increased in the group with multiple PRP injections compared to that in the group with multiple HA injections (p < 0.01) at 3 and 6 months.
Combination with HA
Most studies suggest that combining PRP with HA does not result in a higher efficacy than PRP alone. In 2022, a pooled analysis by Zhang et al. (2022) suggested that combining PRP with HA is not better than injecting PRP alone for treating knee osteoarthritis40. Similarly, the study by Nouri et al. (2022) compared the treatment efficacy of using PRP, HA, and combined PRP + HA for hip osteoarthritis and showed that although all three groups improved in pain and joint function, using PRP or PRP combined with HA resulted in higher efficacy than using HA alone; specifically, there was no enhanced efficacy when combining HA with PRP compared to using PRP alone41.
Location of Osteoarthritis and Injection Site
Osteoarthritis occurs at various locations in the body, but the response to osteoarthritis treatment at different locations varies. Indeed, a recent pooled analysis of 24 randomized controlled trials (RCT) with 1344 patients treated for osteoarthritis at different locations, including the knee (KOA), hip (HOA), ankle (AOA), and temporomandibular joint osteoarthritis (TMJOA)42, showed that PRP injections are safe and effective in improving the function of particular locations, especially the knee (KOA), temporomandibular joint (TMKOA), and ankle osteoarthritis (AOA). However, PRP did not effectively reduce pain in patients with hip osteoarthritis (HOA). This observation was similar to that of a previous study by Dong et al. (2020). This study also showed that PRP injections are effective in reducing pain from knee OA, but not from hip osteoarthritis43. This is why Belk et al. (2022) also reported that injecting LP-PRP into patients with hip osteoarthritis resulted in similar efficacy to HA injection44. However, many comprehensive reports on the treatment effect of PRP in hip arthritis contain biases in data collection based on published summaries45.
In treating knee osteoarthritis, injecting PRP into the joint (intra-articular) and the combination of injecting PRP into the joint along with injection into the bone (intraosseous) does not result in a difference in treatment efficacy. The combination of both joint and bone injections does not provide any benefit over joint injection alone for up to 6 months of follow-up in terms of functional improvement and pain reduction46.
Prognostic Factors in the Efficacy of Treating Osteoarthritis
Although many studies and analyses have shown that PRP is generally effective in treating osteoarthritis, there is still a group of patients who do not respond to treatment with PRP injections. The first study to explore prognostic factors in treatment response to PRP was recently reported by Ota et al. (2024). Although the study had a relatively small number of patients (36 knee joints), the research group showed a tendency for the impact of the Japanese Knee Injury and Osteoarthritis Outcome Score (J-KOOS) and hyperlipidemia syndrome. Surprisingly, those who responded to PRP treatment had lower J-KOOS scores and hyperlipidemia syndromes47.
Cao et al. (2023) used pharmacodynamic maximal effect models and meta-analysis to show that patients with osteoarthritis with higher symptom scores, older age (≥ 60 years), higher BMI (≥ 30), lower Kellgren-Lawrence degeneration degree (≤ 2), and shorter duration of osteoarthritis (< 6 months) had higher treatment efficacy with PRP48.
| PRP characteristics | Suggestions |
| Dose of platelets/joint | > 5.10 9 |
| Volume of PRP/joint | 4-8 mL |
| Type of PRP | Pure PRP or LP-PRP |
| Activation status | Activated PRP |
| Repeated injections | 3 injections (monthly) |
| Knee osteoarthritis grade (Kellgren-Lawrence) | I-III |
Discussion and Suggestions
The effectiveness of PRP treatment for osteoarthritis has been increasingly affirmed by numerous RCT studies and has been analyzed in several recent publications. Its anti-inflammatory and pain-reducing effects and enhancement of cartilage regeneration and osteoarthritis are attributed to the protein content within platelets, especially growth factors and cytokines. While clinical studies have shown the beneficial effects of PRP in treating osteoarthritis, some studies have indicated inconclusive results; hence, many professional associations have yet to officially recognize PRP as a treatment for osteoarthritis, particularly knee osteoarthritis47, 48. The reasons for the inconsistency in clinical treatment outcomes when PRP is used for osteoarthritis have become clearer in recent years. Many pooled analyses to clarify the issues affecting the treatment efficacy of PRP have been published in 2023 and 2024, but this analysis affirms that the treatment effectiveness of PRP for osteoarthritis is influenced by various factors, including platelet count, type of PRP, activation state of PRP, repeat injections, and other prognostic factors. Achieving effective PRP treatment requires the optimization of several factors, and we propose the following optimal protocol for PRP treatment for osteoarthritis:
Patient Selection
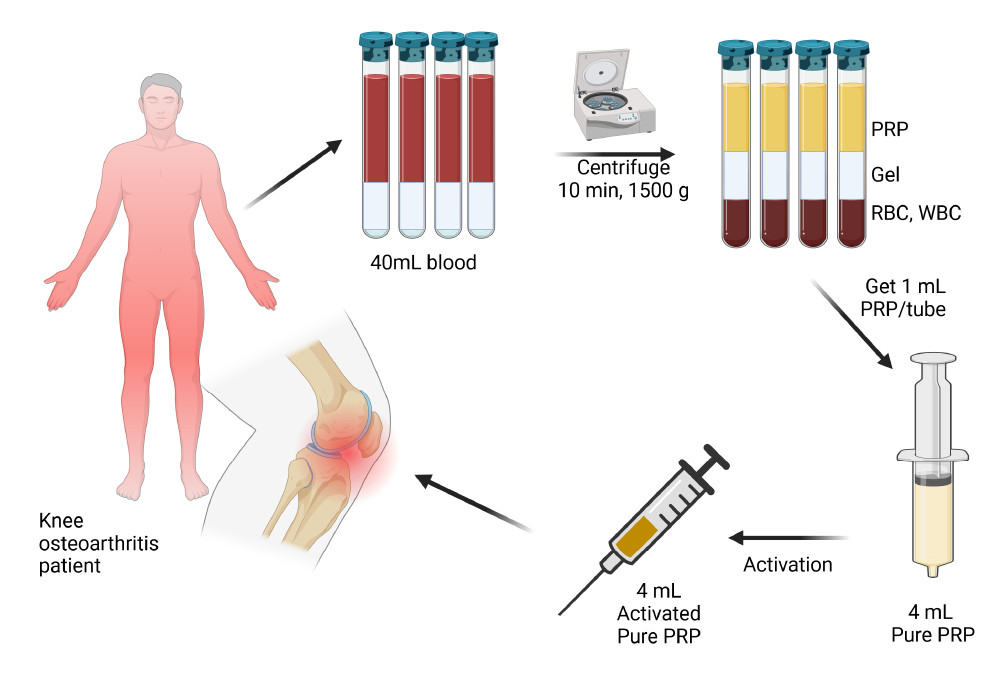
PRP Collection, Processing, and Injection to the Patient
Patient Monitoring After Treatment
Conclusion
Platelet-rich plasma (PRP) is a blood product that contains a significantly larger number of platelets than the normal physiological threshold. As this product contains a large amount of growth factors and cytokines that play roles in inflammation, pain reduction, and stimulation of cell proliferation, PRP is a suitable biological product for treating many injuries. In recent years, studies and analyses based on clinical evidence have confirmed the role of PRP in treating osteoarthritis. The treatment effectiveness of PRP in osteoarthritis is shown to depend on several factors, including platelet count, type of PRP, PRP activation, and injection site, which significantly impact treatment effectiveness. Particularly, in treating knee osteoarthritis, the treatment will be effective when at least 5 billion platelets are used in either activated pure PRP or LP-PRP. With the current evidence, this article once again supports the use of PRP in treating osteoarthritis, especially knee osteoarthritis. We hope that with these advancements, professional associations will soon recognize PRP injections as a treatment method for osteoarthritis diseases.
Abbreviations
22G - Gauge Size for Neediles, AOA - Ankle Osteoarthritis, BMAC - Bone Marrow Aspirate Concentrate, EGF - Epidermal Growth Factor, EQ-VAS - EuroQol Visual Analogue Scale, FGF - Fibroblast Growth Factor, HA - Hyaluronic Acid, HGF - Hepatocyte Growth Factor, HGB - Hemoglobin, HOA - Hip Osteoarthritis, IGF-1, 2 - Insulin-like Growth Factors 1 and 2, IKDC - International Knee Documentation Committee, J-KOOS - Japanese Knee Injury and Osteoarthritis Outcome Score, KOA - Knee Osteoarthritis, LP-PRP - Leukocyte-Poor Platelet-Rich Plasma, LR-PRP - Leukocyte-Rich Platelet-Rich Plasma, NSAID - Non-Steroidal Anti-Inflammatory Drug, PDGF - Platelet-Derived Growth Factor, PRP - Platelet-Rich Plasma, RCTs - Randomized Controlled Trials, TMJOA - Temporomandibular Joint Osteoarthritis, VAS - Visual Analogue Scale, VEGF - Vascular Endothelial Growth Factor, WOMAC - Western Ontario and McMaster Universities Osteoarthritis Index
Acknowledgments
None.
Author’s contributions
All authors equally contributed to this work, read and approved the final manuscript.
Funding
None.
Availability of data and materials
Not applicable.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
-
Alves
R.,
Grimalt
R.,
A Review of Platelet-Rich Plasma: History, Biology, Mechanism of Action, and Classification. Skin Appendage Disorders.
2018;
4
(1)
:
18-24
.
View Article PubMed Google Scholar -
Xiao
Z.,
Chen
W.,
Wei
Z.,
Zhang
Q.,
Tang
G.,
Global trends and hotspots in the application of platelet-rich plasma in knee osteoarthritis: A bibliometric analysis from 2008 to 2022. Medicine.
2023;
102
(47)
.
View Article PubMed Google Scholar -
Paichitrojjana
A.,
Paichitrojjana
A.,
Platelet rich plasma and its use in hair regrowth: a review. Drug Design, Development and Therapy.
2023;
16
:
635-645
.
-
Shimizu
Y.,
Ntege
E.H.,
Sunami
H.,
Current regenerative medicine-based approaches for skin regeneration: A review of literature and a report on clinical applications in Japan. Regenerative therapy.
2022;
21
:
73-80
.
View Article PubMed Google Scholar -
Emer
J.,
Platelet-rich plasma (PRP): current applications in dermatology. Skin therapy letter.
2019;
24
(5)
:
1-6
.
PubMed Google Scholar -
Dominika
E.,
Michal
P.,
Mazur
M.,
Irena
D.,
Platelet-rich plasma and platelet-rich fibrin in oral surgery: A narrative review. Dental and Medical Problems.
2023;
60
(1)
:
177-186
.
View Article PubMed Google Scholar -
Vaidakis
D.,
Papapanou
M.,
Siristatidis
C.S.,
Autologous platelet-rich plasma for assisted reproduction. Cochrane Database of Systematic Reviews.
2024;
4
(4)
:
CD013875
.
View Article Google Scholar -
Sharara
F.I.,
Lelea
L.L.,
Rahman
S.,
Klebanoff
J.S.,
Moawad
G.N.,
A narrative review of platelet-rich plasma (PRP) in reproductive medicine. Journal of Assisted Reproduction and Genetics.
2021;
38
:
1003-1012
.
View Article PubMed Google Scholar -
Liu
S.S.,
Xu
L.L.,
Liu
L.K.,
Lu
S.J.,
Cai
B.,
Platelet-rich plasma therapy for temporomandibular joint osteoarthritis: A randomized controlled trial. Journal of Cranio-Maxillo-Facial Surgery.
2023;
51
(11)
:
668-74
.
View Article PubMed Google Scholar -
Park
Y.B.,
Kim
J.H.,
Ha
C.W.,
Lee
D.H.,
Clinical Efficacy of Platelet-Rich Plasma Injection and Its Association With Growth Factors in the Treatment of Mild to Moderate Knee Osteoarthritis: A Randomized Double-Blind Controlled Clinical Trial As Compared With Hyaluronic Acid. The American Journal of Sports Medicine.
2021;
49
(2)
:
487-96
.
View Article PubMed Google Scholar -
Nouri
F.,
Babaee
M.,
Peydayesh
P.,
Esmaily
H.,
Raeissadat
S.A.,
Comparison between the effects of ultrasound guided intra-articular injections of platelet-rich plasma (PRP), high molecular weight hyaluronic acid, and their combination in hip osteoarthritis: a randomized clinical trial. BMC Musculoskeletal Disorders.
2022;
23
(1)
:
856
.
View Article PubMed Google Scholar -
Chouhan
D.K.,
Dhillon
M.S.,
Patel
S.,
Bansal
T.,
Bhatia
A.,
Kanwat
H.,
Multiple Platelet-Rich Plasma Injections Versus Single Platelet-Rich Plasma Injection in Early Osteoarthritis of the Knee: An Experimental Study in a Guinea Pig Model of Early Knee Osteoarthritis. The American Journal of Sports Medicine.
2019;
47
(10)
:
2300-7
.
View Article PubMed Google Scholar -
Fice
M.P.,
Miller
J.C.,
Christian
R.,
Hannon
C.P.,
Smyth
N.,
Murawski
C.D.,
The Role of Platelet-Rich Plasma in Cartilage Pathology: An Updated Systematic Review of the Basic Science Evidence. Arthroscopy.
2019;
35
(3)
.
View Article PubMed Google Scholar -
Khatab
S.,
van Buul
G.M.,
Kops
N.,
Bastiaansen-Jenniskens
Y.M.,
Bos
P.K.,
Verhaar
J.A.,
Intra-articular Injections of Platelet-Rich Plasma Releasate Reduce Pain and Synovial Inflammation in a Mouse Model of Osteoarthritis. The American Journal of Sports Medicine.
2018;
46
(4)
:
977-86
.
View Article PubMed Google Scholar -
Mariani
E.,
Roffi
A.,
Cattini
L.,
Pulsatelli
L.,
Assirelli
E.,
Krishnakumar
G.S.,
Release kinetic of pro- and anti-inflammatory biomolecules from platelet-rich plasma and functional study on osteoarthritis synovial fibroblasts. Cytotherapy.
2020;
22
(7)
:
344-53
.
View Article PubMed Google Scholar -
Moussa
M.,
Lajeunesse
D.,
Hilal
G.,
El Atat
O.,
Haykal
G.,
Serhal
R.,
Platelet rich plasma (PRP) induces chondroprotection via increasing autophagy, anti-inflammatory markers, and decreasing apoptosis in human osteoarthritic cartilage. Experimental Cell Research.
2017;
352
(1)
:
146-56
.
View Article PubMed Google Scholar -
Watson
S.P.,
Bahou
W.F.,
Fitzgerald
D.,
Ouwehand
W.,
Rao
A.K.,
Leavitt
A.D.,
Platelet Physiology Subcommittee
ISTH,
Mapping the platelet proteome: a report of the ISTH Platelet Physiology Subcommittee. Journal of Thrombosis and Haemostasis.
2005;
3
(9)
:
2098-101
.
View Article PubMed Google Scholar -
Belk
J.W.,
Lim
J.J.,
Keeter
C.,
McCulloch
P.C.,
Houck
D.A.,
McCarty
E.C.,
Patients With Knee Osteoarthritis Who Receive Platelet-Rich Plasma or Bone Marrow Aspirate Concentrate Injections Have Better Outcomes Than Patients Who Receive Hyaluronic Acid: Systematic Review and Meta-analysis. Arthroscopy.
2023;
39
(7)
:
1714-34
.
View Article PubMed Google Scholar -
Veronesi
F.,
Andriolo
L.,
Salerno
M.,
Boffa
A.,
Giavaresi
G.,
Filardo
G.,
Adipose Tissue-Derived Minimally Manipulated Products versus Platelet-Rich Plasma for the Treatment of Knee Osteoarthritis: A Systematic Review of Clinical Evidence and Meta-Analysis. Journal of Clinical Medicine.
2023;
13
(1)
:
67
.
View Article PubMed Google Scholar -
Qiao
X.,
Yan
L.,
Feng
Y.,
Li
X.,
Zhang
K.,
Lv
Z.,
Efficacy and safety of corticosteroids, hyaluronic acid, and PRP and combination therapy for knee osteoarthritis: a systematic review and network meta-analysis. BMC Musculoskeletal Disorders.
2023;
24
(1)
:
926
.
View Article PubMed Google Scholar -
Khalid
S.,
Ali
A.,
Deepak
F.,
Zulfiqar
M.S.,
Malik
L.U.,
Fouzan
Z.,
Comparative effectiveness of intra-articular therapies in knee osteoarthritis: a meta-analysis comparing platelet-rich plasma (PRP) with other treatment modalities. Annals of Medicine and Surgery (London).
2023;
86
(1)
:
361-72
.
View Article PubMed Google Scholar -
Wang
R.,
Xie
Y.,
Xie
L.,
Liu
J.,
Jia
J.,
Chen
X.,
Platelet-rich plasma versus corticosteroid in the treatment of knee osteoarthritis: a systematic review and meta-analysis of randomized controlled trials. Georgian Medical News.
2024;
2024
(349)
:
169-82
.
PubMed Google Scholar -
Oeding
J.F.,
Varady
N.H.,
Fearington
F.W.,
Pareek
A.,
Strickland
S.M.,
Nwachukwu
B.U.,
Platelet-Rich Plasma Versus Alternative Injections for Osteoarthritis of the Knee: A Systematic Review and Statistical Fragility Index-Based Meta-analysis of Randomized Controlled Trials. The American Journal of Sports Medicine.
2024;
\textbullet\textbullet\textbullet
.
View Article PubMed Google Scholar -
Gesheff
M.G.,
Scalzitti
D.A.,
Bains
S.S.,
Dubin
J.,
Delanois
R.E.,
Time to Total Knee Arthroplasty (TKA) Post Intra-Articular Injection. Journal of Clinical Medicine.
2024;
13
(13)
:
3764
.
View Article PubMed Google Scholar -
Hohmann
E.,
Editorial Commentary: High-Platelet-Dose Platelet-Rich Plasma May Be the Nonoperative Treatment of Choice for Knee Osteoarthritis. Arthroscopy.
2024;
S0749-8063
(24)
:
00269-X
.
View Article PubMed Google Scholar -
Patel
S.,
Gahlaut
S.,
Thami
T.,
Chouhan
D.K.,
Jain
A.,
Dhillon
M.S.,
Comparison of Conventional Dose Versus Superdose Platelet-Rich Plasma for Knee Osteoarthritis: A Prospective, Triple-Blind, Randomized Clinical Trial. Orthopaedic Journal of Sports Medicine.
2024;
12
(2)
.
View Article PubMed Google Scholar -
Berrigan
W.A.,
Bailowitz
Z.,
Park
A.,
Reddy
A.,
Liu
R.,
Lansdown
D.,
A Greater Platelet Dose May Yield Better Clinical Outcomes for Platelet-Rich Plasma in the Treatment of Knee Osteoarthritis: A Systematic Review. Arthroscopy.
2024
.
View Article Google Scholar -
Bennell
K.L.,
Paterson
K.L.,
Metcalf
B.R.,
Duong
V.,
Eyles
J.,
Kasza
J.,
Effect of Intra-articular Platelet-Rich Plasma vs Placebo Injection on Pain and Medial Tibial Cartilage Volume in Patients With Knee Osteoarthritis: The RESTORE Randomized Clinical Trial. Journal of the American Medical Association.
2021;
326
(20)
:
2021-30
.
View Article PubMed Google Scholar -
Bansal
H.,
Leon
J.,
Pont
J.L.,
Wilson
D.A.,
Bansal
A.,
Agarwal
D.,
Platelet-rich plasma (PRP) in osteoarthritis (OA) knee: correct dose critical for long term clinical efficacy. Scientific Reports.
2021;
11
(1)
:
3971
.
View Article PubMed Google Scholar -
Xiong
Y.,
Gong
C.,
Peng
X.,
Liu
X.,
Su
X.,
Tao
X.,
Efficacy and safety of platelet-rich plasma injections for the treatment of osteoarthritis: a systematic review and meta-analysis of randomized controlled trials. Frontiers in Medicine.
2023;
10
.
View Article PubMed Google Scholar -
Kim
J.H.,
Park
Y.B.,
Ha
C.W.,
Are leukocyte-poor or multiple injections of platelet-rich plasma more effective than hyaluronic acid for knee osteoarthritis? A systematic review and meta-analysis of randomized controlled trials. Archives of Orthopaedic and Trauma Surgery.
2023;
143
(7)
:
3879-97
.
View Article PubMed Google Scholar -
Kim
J.H.,
Park
Y.B.,
Ha
C.W.,
Roh
Y.J.,
Park
J.G.,
Adverse Reactions and Clinical Outcomes for Leukocyte-Poor Versus Leukocyte-Rich Platelet-Rich Plasma in Knee Osteoarthritis: A Systematic Review and Meta-analysis. Orthopaedic Journal of Sports Medicine.
2021;
9
(6)
:
23259671211011948
.
View Article PubMed Google Scholar -
Chen
L.,
Jin
S.,
Yao
Y.,
He
S.,
He
J.,
Comparison of clinical efficiency between intra-articular injection of platelet-rich plasma and hyaluronic acid for osteoarthritis: a meta-analysis of randomized controlled trials. Therapeutic advances in musculoskeletal disease.
2023;
2023
(15)
:
1759720X231157043
.
View Article PubMed Google Scholar -
Abbas
A.,
Du
J.T.,
Dhotar
H.S.,
The Effect of Leukocyte Concentration on Platelet-Rich Plasma Injections for Knee Osteoarthritis: A Network Meta-Analysis. The Journal of Bone and Joint Surgery. American Volume.
2022;
104
(6)
:
559-70
.
View Article PubMed Google Scholar -
Simental-Mendía
M.,
Ortega-Mata
D.,
Tamez-Mata
Y.,
Olivo
C.A.,
Vilchez-Cavazos
F.,
Comparison of the clinical effectiveness of activated and non-activated platelet-rich plasma in the treatment of knee osteoarthritis: a systematic review and meta-analysis. Clinical Rheumatology.
2023;
42
(5)
:
1397-408
.
View Article PubMed Google Scholar -
Tao
X.,
Aw
A.A.,
Leeu
J.J.,
Bin Abd Razak
H.R.,
Three Doses of Platelet-Rich Plasma Therapy Are More Effective Than One Dose of Platelet-Rich Plasma in the Treatment of Knee Osteoarthritis: A Systematic Review and Meta-analysis. Arthroscopy.
2023;
39
(12)
.
View Article PubMed Google Scholar -
Zhuang
W.,
Li
T.,
Li
Y.,
Zhang
Y.,
Gao
J.,
Wang
X.,
The varying clinical effectiveness of single, three and five intraarticular injections of platelet-rich plasma in knee osteoarthritis. Journal of Orthopaedic Surgery and Research.
2024;
19
(1)
:
284
.
View Article PubMed Google Scholar -
Saraf
A.,
Hussain
A.,
Bishnoi
S.,
Habib
H.,
Garg
A.,
Serial intraarticular injections of growth factor concentrate in knee osteoarthritis: A placebo controlled randomized study. Journal of Orthopaedics.
2023;
37
:
46-52
.
View Article PubMed Google Scholar -
Li
S.,
Xing
F.,
Yan
T.,
Zhang
S.,
Chen
F.,
Multiple Injections of Platelet-Rich Plasma Versus Hyaluronic Acid for Knee Osteoarthritis: A Systematic Review and Meta-Analysis of Current Evidence in Randomized Controlled Trials. Journal of Personalized Medicine.
2023;
13
(3)
:
429
.
View Article PubMed Google Scholar -
Zhang
Q.,
Liu
T.,
Gu
Y.,
Gao
Y.,
Ni
J.,
Efficacy and safety of platelet-rich plasma combined with hyaluronic acid versus platelet-rich plasma alone for knee osteoarthritis: a systematic review and meta-analysis. Journal of Orthopaedic Surgery and Research.
2022;
17
(1)
:
499
.
View Article PubMed Google Scholar -
Dong
Y.,
Zhang
B.,
Yang
Q.,
Zhu
J.,
Sun
X.,
The effects of platelet-rich plasma injection in knee and hip osteoarthritis: a meta-analysis of randomized controlled trials. Clinical Rheumatology.
2021;
40
(1)
:
263-77
.
View Article PubMed Google Scholar -
Belk
J.W.,
Houck
D.A.,
Littlefield
C.P.,
Kraeutler
M.J.,
Potyk
A.G.,
Mei-Dan
O.,
Platelet-Rich Plasma Versus Hyaluronic Acid for Hip Osteoarthritis Yields Similarly Beneficial Short-Term Clinical Outcomes: A Systematic Review and Meta-analysis of Level I and II Randomized Controlled Trials. Arthroscopy.
2022;
38
(6)
:
2035-46
.
View Article PubMed Google Scholar -
Kim
D.,
Bashrum
B.S.,
Kotlier
J.L.,
Mayfield
C.K.,
Thompson
A.A.,
Abu-Zahra
M.,
Reporting Bias is Highly Prevalent in Systematic Reviews and Meta-Analyses of Platelet Rich Plasma Injections for Hip Osteoarthritis. Arthroscopy, Sports Medicine, and Rehabilitation.
2024;
6
(1)
.
View Article PubMed Google Scholar -
Barman
A.,
Prakash
S.,
Sahoo
J.,
Mukherjee
S.,
Maiti
R.,
Roy
S.S.,
Single intra-articular injection with or without intra-osseous injections of platelet-rich plasma in the treatment of osteoarthritis knee: A single-blind, randomized clinical trial. Injury.
2022;
53
(3)
:
1247-53
.
View Article PubMed Google Scholar -
Ota
M.,
Okumo
T.,
Sato
A.,
Nagasaka
R.,
Mukunoki
M.,
Izukashi
K.,
Prognostic Factors in Intra-articular Platelet-Rich Plasma Treatment for Knee Osteoarthritis: A Comparative Analysis of Responders and Nonresponders. Cureus.
2024;
16
(4)
.
View Article PubMed Google Scholar -
Cao
Y.,
Luo
J.,
Han
S.,
Li
Z.,
Fan
T.,
Zeng
M.,
A model-based quantitative analysis of efficacy and associated factors of platelet rich plasma treatment for osteoarthritis. International Journal of Surgery.
2023;
109
(6)
:
1742-52
.
View Article PubMed Google Scholar -
Bannuru
R.R.,
Osani
M.C.,
Vaysbrot
E.E.,
Arden
N.K.,
Bennell
K.,
Bierma-Zeinstra
S.M.,
OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthritis and Cartilage.
2019;
27
(11)
:
1578-89
.
View Article PubMed Google Scholar -
Kolasinski
S.L.,
Neogi
T.,
Hochberg
M.C.,
Oatis
C.,
Guyatt
G.,
Block
J.,
2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand, Hip, and Knee. Arthritis Care & Research (Hoboken).
2020;
72
(2)
:
149-62
.
View Article PubMed Google Scholar
Comments
Article Details
Volume & Issue : Vol 11 No 7 (2024)
Page No.: 6556-6564
Published on: 2024-07-31
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 5140 times
- PDF downloaded - 1092 times
- XML downloaded - 136 times
 Biomedpress
Biomedpress



