Abstract
Background: Chronic myeloid leukaemia is a form of myeloproliferative neoplasm characterised by the proliferation of granulocytes. This particular form of myeloproliferative neoplasm is rare, accounting for approximately 2% – 3% of recently diagnosed pediatric leukaemia. Neuropsychological manifestation is a rare initial sign in patients with chronic myeloid leukaemia.
Case presentation: A 10-year-old girl who presented with two weeks of abnormal behaviour. Her neurological assessment revealed no abnormality. Her serial full blood count revealed persistent leucocytosis, and her most recent full blood picture showed 2.3% blast cells. Following a comprehensive analysis of bone marrow smear and identification of the BCR-ABL fusion gene, it was concluded that the patient had chronic myeloid leukaemia in chronic-phase. Her neuropsychological symptoms improved after a few months of imatinib treatment, and she will be scheduled for a stem cell transplant if her human leukocyte antigen matches those of other siblings.
Conclusion: Neuropsychological manifestations in chronic myeloid leukaemia-chronic phase are uncommon in children and can be mistaken for more prevalent conditions. Physicians should maintain a vigilant stance due to the distinct management and prognosis of chronic myeloid leukaemia in comparison to the more prevalent condition in paediatric.
Introduction
Chronic myeloid leukemia (CML) is rare in children and adolescents. It represents 2% - 3% of all pediatric leukemia1. Classically, CML is classified into three phases of progression: chronic, accelerated, and blastic2. Eighty-five percent of cases are diagnosed as CML-chronic phase (CP)2. CML-CP typically progresses to the accelerated phase (AP) and blast phase (BP) within 3-5 years3. The most common symptoms of CML-CP include fatigue, weight loss, abdominal fullness, hemorrhage, purpura, splenomegaly, leukocytosis, anemia, and thrombocytosis1. Nevertheless, no case of neuropsychological manifestation as an initial presentation of CML-CP in pediatrics has been reported. The atypical presentation gives rise to a diagnostic conundrum, leaving both the diagnosis and treatment uncertain.
Case Report
A 10-year-old girl with underlying clinical Goldenhar syndrome presented with abnormal behavior for one week. It was characterized as erupting in uncontrollable screams and tears. Furthermore, she encountered visual and auditory hallucinations. She recounted seeing a black shadow behind her and hearing extra voices when there were no other people nearby. The symptoms were preceded by three days of fever. She did not have photophobia, vomiting, constitutional symptoms, or seizures. On examination, she was alert, comfortable, not septic-looking, and her Glasgow Coma Scale was 15/15. Vital signs were normal. Abdominal palpation revealed no hepatosplenomegaly. Neurological examination was normal. Initial laboratory analysis revealed leukocytosis, as evidenced by a white cell count (WCC) of 27 x 109/L, in conjunction with normal hemoglobin and platelet counts (Table 1). The analysis of cerebrospinal fluid (CSF) revealed no organism growth and normal biochemistry. She was diagnosed with clinical meningoencephalitis. A combination of intravenous (IV) ceftriaxone and acyclovir was initiated. The neuropsychological symptom persisted even after treatment. Consequently, she was referred to a child psychologist for behavioral modification. Brain magnetic resonance imaging (MRI) revealed the presence of normal brain morphology. Before she was discharged, her serial WCC had increased to 31 x 109/L (Table 1). However, because she remained hemodynamically stable she was discharged after 14 days of antibiotic treatment. She was followed up in the pediatric clinic due to persistent leukocytosis. A serial full blood picture (FBP) analysis revealed an infection.
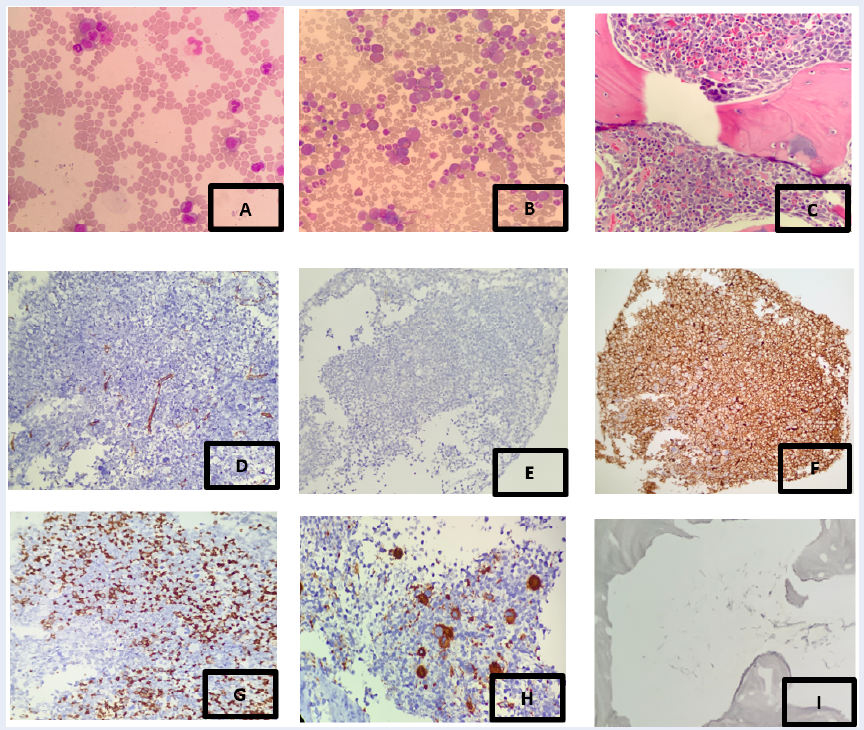
She remained well for four months before her readmission for an upper respiratory tract infection. Despite receiving treatment from a child psychologist, her abnormal behavior persisted. Her serial WCC (Table 1) revealed leukocytosis that had increased to 114 x 109/L. Repeated FBP revealed persistent leukocytosis with the presence of 2.3% blast cells and thrombocytosis, highly suspicious of hematological disorders, to rule out myelodysplastic syndrome or myeloproliferative neoplasm (Figure 1). She was therefore subjected to bone marrow aspiration and trephine biopsy (BMAT) (Figure 1). The results were consistent with a myeloproliferative neoplasm, unable to exclude CML. Consequently, molecular cytogenetic analysis (FISH) was performed, which identified abnormal metaphases in all cells examined, showing a reciprocal translocation between segment of chromosome 9 to 9q34 and a segment of chromosome 22 distal to 22q11.2, resulting in the BCR-ABL1 fusion gene (Philadelphia chromosome). This result is consistent with the clinical diagnosis of CML. CSF analysis revealed the absence of blast cells in the spinal fluid. Hydroxyurea and imatinib were administered to the patient, and she has been compliant with the medication. The neuropsychiatric manifestation was controlled and improving. The most recent FBP revealed a normal WCC with no blast cells. BMA will be repeated according to the treatment guidelines. Human leukocyte antigen (HLA) testing was performed on her and her siblings in preparation for a stem cell transplant (SCT).
| 23 rd February 2023 | 26 th February 2023 | 26 th June 2023 | 20 th September 2023 | |
|---|---|---|---|---|
| Full Blood Count WCC (10 9 /L) | 27.05 | 31.42 | 114 | 12.96 |
| Haemoglobin (g/dL) | 13 | 14.9 | 12.4 | 11.9 |
| Platelet (10 9 /L) | 479 | 621 | 575 | 443 |
Discussion
Pediatric CML is a malignant disease characterized by granulocyte aberrant hyperplasia produced by pluripotent stem cell cloning4. It rarely affects children and generally progresses in three stages: chronic, accelerated, and blast. The initial clinical manifestation of splenomegaly with leukocytosis in generally healthy children raises the possibility of CML-CP5. Typical clinical manifestations of CML during CP include malaise, lethargy, fever, night sweats, weakness, and symptoms associated with splenomegaly and platelet dysfunction-related bleeding6. A child may also manifest intermittent headaches, visual impairments, and priapism as a result of hyperleukocytosis6. Along with these symptoms, children diagnosed with the accelerated phase (AP) disease also exhibit lymphadenopathy, cutaneous involvement, rapidly progressing systemic symptoms, and splenomegaly1, 7. CML-BP resembles acute leukemia in its clinical presentation2. A limited number of cases have documented neurological manifestations in CML during BP rather than CP, which result from blast cell metastasis8. In our case, the diagnosis was delayed even though she had been admitted and followed up due to hyperleukocytosis. Initially, a suspected case of clinical meningoencephalitis was linked to a neuropsychological presentation. Additional tests, like FBP and brain MRI, showed no malignant cells and normal brain anatomy, even though the child had persistent neuropsychiatric symptoms and isolated leukocytosis. This made it more challenging to make a diagnosis. Moreover, no correlation has been observed between Goldenhar syndrome and CML. CML is known to be associated with Sweet’s syndrome (acute febrile neutrophilic dermatosis) and Down syndrome. Due to the rarity of the association and the atypical initial manifestation of CML, the diagnosis of CML was not considered during her initial presentation, resulting in uncertain treatment. To solve the diagnosis dilemma in this case, we should proceed with an early BMA instead of serial FBP, which was normal as the patient had persistent leukocytosis with no obvious causes.
The precise mechanisms underlying the progression of BP in children with CML remain unknown; nevertheless, they are believed to be similar to those observed in adults4. Due to the tyrosine kinase activity inherent to both components, the Philadelphia (Ph1) chromosome and the resulting BCR-ABL1 fusion gene induce granulocytic and blast proliferation in leukemic stem cells5. This is partly because BCR-ABL1 inhibits c-Jun from working, a transcription factor that aids in the transformation of blasts and CML neutrophils into monoclonuclear cells5. Consequently, the BCR-ABL1 fusion gene should be found in mature neutrophils in CML instead of blasts in de novo AML5. The presence of the BCR-ABL1 fusion gene also causes mature eosinophils and basophils to proliferate in CML1, 2. It is critical to distinguish CML-BP from AML with BCR-ABL1, as the two conditions require distinct treatment approaches. A tyrosine kinase inhibitor is administered in conjunction with an early allogeneic stem cell transplant to treat CML-BP, whereas intensive induction chemotherapy is used to treat AML with BCR-ABL1. Existing tyrosine kinase inhibitors often produce unfavorable results, and the average survival time following the diagnosis of CML-BP is less than one year8. The EUTOS Long-Term Survival (ELTS) score was better at differentiating between progression-free survival and other scores in children and adolescents with CML than the SOKAL, Hasford, and EUTOS scores7.
In the interim between the initiation of tyrosine kinase inhibitors (TKI) and the initial treatment of pediatric CML, hydroxyurea is frequently administered to patients with elevated WCC7. Allopurinol should be administered to patients who have a significant tumor burden7. TKI is currently the treatment of choice for patients with chronic-phase CML7. In addition to targeting the BCR-ABL1 fusion protein, TKIs may also inhibit other tyrosine kinases such as platelet-derived growth factor receptor (PDGFR), vascular endothelial growth factor receptors (VEGFR), c-KIT, and others that share pathways for bone growth and metabolism, as well as other endocrine functions5. The long-term effects of TKIs on developing children are currently unknown and are expected to differ from what is observed in adults. While safer and more innovative treatments are being pursued for CML in children, it is crucial to define the safety and efficacy of existing TKIs in this population. The only TKI approved by the FDA as a first-line treatment for children with CML was imatinib7. As a potent and selective inhibitor of BCR-ABL tyrosine kinase, imatinib is the preferred treatment for chronic CML. Furthermore, it has demonstrated efficacy during the accelerated and blastic phases of CML. Nonetheless, numerous investigations have demonstrated that the drug and its metabolites have limited CNS penetration6. Targeted BCR/ABL1 tyrosine kinase inhibitors of the second generation, including dasatinib and nilotinib, penetrate the blood-brain barrier more efficiently1. Critical monitoring occurs during the initial one to two years of treatment, when the majority of scenarios of primary and secondary resistance are identified5. After patients have attained and sustained a significant molecular response for 12 months, the likelihood of progression is exceedingly minimal, thereby diminishing the importance of monitoring. In our case, she will undergo additional BMA and molecular testing to evaluate the efficacy of the treatment. There is a lack of treatment recommendations pertaining to CML involving the central nervous system. Aggressive treatment options in pediatric CML include systemic and intrathecal chemotherapy, radiotherapy, and allogeneic stem cell transplantation6. Nevertheless, allogeneic stem cell transplantation stands as the sole therapeutic approach that has demonstrated efficacy in curing this illness7.
This case report presents a unique case, but it is limited by the inherent constraints of a case report. To better understand the prevalence and characteristics of similar atypical presentations of CML, further investigation through larger and more robust study designs, such as case series or observational studies, would be warranted. These types of studies could provide more comprehensive insights into the occurrence and features of these atypical CML presentations.
Conclusion
Neuropsychological manifestation in CML-CP is a rare presentation in the pediatric population that mimics more prevalent diseases in that age group, such as meningitis, encephalitis, and solid brain tumors. Physicians should maintain a high index of suspicion because both the treatment and prognosis for CML differ from those of these other diseases.
Abbreviations
AP - Accelerated Phase, BMA - Bone Marrow Aspirate, BMAT - Bone Marrow Aspiration and Trephine Biopsy, BMT - Bone Marrow Trephine Biopsy, BP - Blast Phase, CML - Chronic Myeloid Leukemia, CNS - Central Nervous System, CSF - Cerebrospinal Fluid, ELTS - EUTOS Long-Term Survival, FBP - Full Blood Picture, FDA - Food and Drug Administration, FISH - Fluorescence In Situ Hybridization, HLA - Human Leukocyte Antigen, IHC - Immunohistochemistry, IV - Intravenous, MPO - Myeloperoxidase, MRI - Magnetic Resonance Imaging, PDGFR - Platelet-Derived Growth Factor Receptor, PBF - Peripheral Blood Film, SCT - Stem Cell Transplant, TKI - Tyrosine Kinase Inhibitor, VEGFR - Vascular Endothelial Growth Factor Receptors, WCC - White Cell Count, WHO - World Health Organization
Acknowledgments
We extend our gratitude to the patients and their families for their generous contributions to this study. Additionally, we would like to express our appreciation to the director of Hospital Universiti Sains Malaysia for the support in completing the case report.
Author’s contributions
AMMK, NM, AN and NANA participate in drafting the case report. MNH, RHZ, RB and RH are creating the outline of the case. All authors read and approved the final manuscript.
Funding
None.
Availability of data and materials
None.
Ethics approval and consent to participate
None.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
References
-
Pushpam
D.,
Bakhshi
S.,
Paediatric chronic myeloid leukaemia: is it really a different disease?. The Indian Journal of Medical Research.
2019;
149
(5)
:
600-9
.
View Article PubMed Google Scholar -
Hijiya
N.,
Schultz
K.R.,
Metzler
M.,
Millot
F.,
Suttorp
M.,
Perspectives Pediatric chronic myeloid leukemia is a unique disease that requires a different approach. Blood.
2016;
127
(4)
:
391-9
.
View Article Google Scholar -
Dey
B.,
Dutta
A.,
Pediatric chronic myeloid leukemia in myeloid blast crisis. Autopsy and Case Reports.
2023;
13
:
e2023426
.
View Article PubMed Google Scholar -
Syamsuddin
I.K.,
Notopuro
P.B.,
Sensorineural Hearing Loss in Juvenile CML: A Rare Case Report in Surabaya, Indonesia. International Medical Case Reports Journal.
2022;
15
:
367-71
.
View Article PubMed Google Scholar -
Sembill
S.,
Ampatzidou
M.,
Chaudhury
S.,
Dworzak
M.,
Kalwak
K.,
Karow
A.,
Management of children and adolescents with chronic myeloid leukemia in blast phase: international pediatric CML expert panel recommendations. Leukemia.
2023;
37
(3)
:
505-17
.
View Article PubMed Google Scholar -
Boudiaf
H.,
Ezziane
K.,
Rouis
N.O.,
Himrane
M.,
Hakem
S.,
Benchabane
H.,
Isolated blast crisis relapse in the central nervous system of a patient treating for a chronic myelogenous leukemia. The Pan African Medical Journal.
2020;
36
:
142
.
View Article PubMed Google Scholar -
Athale
U.,
Hijiya
N.,
Patterson
B.C.,
Bergsagel
J.,
Andolina
J.R.,
Bittencourt
H.,
Management of chronic myeloid leukemia in children and adolescents: Recommendations from the Children's Oncology Group CML Working Group. Pediatric Blood & Cancer.
2019;
66
(9)
:
e27827
.
View Article PubMed Google Scholar -
Jo
S.,
Yoo
J.W.,
Kim
S.,
Lee
J.W.,
Im
S.A.,
Cho
B.,
Case report: first report of isolated central nervous system lymphoblastic crisis in a child with chronic myeloid leukemia on dasatinib therapy. Frontiers in Oncology.
2023;
13
:
1122714
.
View Article PubMed Google Scholar
Comments
Article Details
Volume & Issue : Vol 11 No 9 (2024)
Page No.: 6792-6796
Published on: 2024-09-30
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
- HTML viewed - 1601 times
- PDF downloaded - 642 times
- XML downloaded - 77 times
 Biomedpress
Biomedpress


